I guess I should have waited one more day before making my previous post because on 15 December I got my catheter removed - and I say a big "Hooray!!" for that! - and then I got even better news:
I got a copy of the histopathology report on the biopsy of my removed prostate and, assuming I am reading it and understanding it correctly, it suggests that the cancer was entirely contained within the prostate and was therefore removed from my body. That is, there is a very good chance that I am effectively "cured" of cancer!
I'll know more when I have a blood test in four weeks or so. At that time, my PSA should be zero (or, at least, very, very low). Assuming that's the case, I'll still have my PSA periodically checked for several years to be sure.
As you might imagine, I was pretty happy to receive this news!
I'll repeat the main part of the histopathology report here and maybe one of my medical friends (Peter? Mike? Kim? Robert? Gina?) can let me know if there's something important I'm missing:
Histological type: Acinar adenocarcinoma
Tumour location:
Dominant nodule - Central anterior, extending into left and right lobes and spanning from upper to lower prostate including the apex.
Non-dominant (>10mm) nodules - Right posterior mid to lower prostate and apex;
Left posterior mid to lower prostate and apex.
Volume of dominant nodule: 3.84 cu cm
Volume of non-dominant nodules: right 0.43 cu cm, left 2.95 cu cm
Gleason score (ISUP 2005): 3+4=7 (all nodules)
Tumour stage: pT2c
Extra-prostatic extension: Absent
Surgical margins: Negative for cancer
Seminal vesicles: Not involved
Lymphovascular invasion: Absent
Perineural invasion: Present
Prostatic intraepithelial neoplasia: Present
Neurovascular bundles: Absent bilaterally
My main area of concern is "Perineural invasion: Present". Wikipedia tells me "perineural invasion, abbreviated PNI, refers to cancer spreading to the space surrounding a nerve." So I'm wondering if this has to do with nerves that were removed as part of the prostate, or if it refers to the nerves that the "nerve-sparing" surgery left inside of me. I'm assuming that it's something like the former, but I'll get more information when I see my urologist/surgeon in four weeks or so. (Or one of my more knowledgeable readers will provide more insight...)
Anyway, it's great to know that it's likely that we have obtained the desired result! Long(er) life, here I come!
Monday 19 December 2011
Wednesday 14 December 2011
I've had my surgery, I'm back home, and things are "OK"
My surgery happened on 8 December and it seemed to go well. I was discharged from the hospital on 11 December. I will now be recovering at home, as well as dealing with the more long-term effects of the surgery, for the next six weeks.
So far, it is going well, in that I am able to get around on my own - albeit slowly and carefully - and there is almost no pain (just some discomfort from having an incision across my abdomen). Every day I have felt a little bit better and I remain basically hopeful and optimistic about the future. I hope that I am now "cured" of my prostate cancer - because we have removed it all from my body - but will probably not know anything more definitive until my follow-up appointment with the surgeon/urologist in about six weeks. The story goes on...(as always).
It has taken me three days of being back at home to finally get this blog entry written. That's partly because I have been focusing strongly on just relaxing/recovering and keeping up with my medications and post-operation procedures, and partly because, as you already know, it takes me a long time to actually get anything composed/written (sigh). As usual, my apologies for the delay (if you were waiting for a post-surgery update).
So that's pretty much the main news. The rest of this post is Other Notes about my time in the hopsital, my condition, and possibilities for the future:
- On 8 December, Ann and I arrived at the hospital for my admission at 6:30 AM, as instructed. (Many thanks to Tee for getting up so early and watching Zuperfliegen so that Ann could attend!) I was taken into surgery at 12:30 PM! It turns out they have all the morning surgery patients come in at the same time - so they have flexibility if they need to shuffle the schedule - and I was apparently pretty close to the bottom of the list. So the most effective method for the hospital was for me to get up early and sit around for six hours? Perhaps this is a function of being treated in the "public" health system.
- Ann and I had been told that the surgery would be 2-3 hours in duration. But I came out of the anaesthetic around 6:00 PM, suggesting that it may have actually lasted about 5 hours! I don't begrudge the medical personnel this difference; I wanted them to be able to do whatever they needed, no matter how long it took. Still, it was a little odd, and it made Ann anxious that no updates were coming when she expected them.
- I got to see my surgeon/urologist shortly before being taken into the operating theatre. He was the first one I saw when I was initially referred to a specialist for my suspicious PSA levels. At the time of my surgery, I had not seen him for a couple of months or more. I asked him about the difference in the plan for my lymph nodes. Specifically: When I first saw him as a private patient, his plan was to remove my lymph nodes (for further analysis of whether the cancer had spread past the prostate), as well as do a nerve-sparing surgery. But when I thought I might have a "robotic" surgery done, I was referred to his collegaue, who thought my lymph nodes should not be removed, and I should not have a nerve-sparing surgery. The fact that the two experts held diametrically opposed views on these issues was unsettling! Then, when I balked at the potential cost of private surgery, they referred me to the clinical trial and I was randomly assigned to the first/original urologist and told that my lymph nodes would not be removed, but he would do the nerve-sparing surgery. So when I asked him about this before the surgery, he said the clinical trial has protocols it has to follow; and that there was probably a 2% chance that cancer had spread to the lymph nodes, but possibly a greater percentage of there being unwanted complications if we removed them. It all sounded to me a little like "we give you the answer that best matches the current version of the situation". Which is potentially problematic, but it does underscore the uncertainties that exist with cancer and surgery in general. And, ultimately, as the patient, you have to do the best research you can so you can make the best decision you can; and then it still comes down to putting yourself in the care of the surgeon and hoping/assuming/believing that he or she will do the best they can and that will be enough.
- The surgeon also casually mentioned that I might need radiotherapy treatments later, because of the nerve-sparing surgery. um...WHAT? The idea is that the nerves being spared are wrapped around the prostate; so the surgeon leaves the outer layer of the prostate such that the nerves still have tissue to cling to and are not irreparably damaged. But if the remaining tissue has cancer cells, then I've still got a problem. This is what "positive margins" means in the analysis of my removed prostate. If the outer edge (margin) of the removed prostate is positive for cancer cells, then it is likely they are also still in the unremoved tissue and further treatment - radiation therapy, in this case - is called for. I knew all of this from my original consultation, I guess; but the emphasis for months has been on "we remove the prostate and cure the cancer!" and it was a little weird to be told/reminded that I may have to go through another involved/invasive procedure at some point in the future. Oh well, like I said: the story goes ever on...
- Coming out of the anesthetic and then getting an occasional self-administered dose of morphine made the first evening/night a bit weird. I believe I was reasonably aware and I think I remember pretty much everything, but I just couldn't keep my eyes open. I was not thrilled with the woozy, out-of-control experience. Once I realized that the morphine contributed to that, I decided to totally stop using it. (I didn't really need it, as the discomfort was minimal.). When I woke up the next morning (9 December), I thought, "Ah, now I'm really awake!"
- On 9 December (the day after my surgery), the registrar (essentially co-surgeon or assistant surgeon) for my operation stopped by and said that everything went swimmingly. I think that's probably true, but I also thought "Well, of course you're going to say that...". She also said that I would probably be discharged the next morning.
- However, despite 9 December being a pretty good recovery day (in that I was able to get out of bed and walk), on the morning of 10 December my blood pressure dropped low again and I got a bit dizzy when I tried to stand. My blood pressure is typically lowish, but it dropped down even lower than usual. So the doctors decided to keep me for another day for observation. That was disappointing and frustrating, as I was planning to go home. However, in hindsight, it was probably for the best. That was not a very good day, though, with me just able to lie in my bed.
- 11 December was much better. I slept well the night before, I felt much better in the morning, my blood pressure returned to normal-ish, and I was able to walk well enough. So I got to go home!
- In typing the above, it sounds like I had a lot to complain about. That's not really true, though. The above points are just some of the key items I had to think about. In general, I was pretty impressed with the professionalism and competence of the many medical professionals that attended to me. It's just that recovery in general, and hospital stays in particular (when you are, after all, the most unwell) are not typically fun experiences.
- It was great having Ann, and often Zuperfliegen, come visit me, of course. It's probably just as well there weren't other visitors, though, as it was a shortish hospital stay and I was somewhat wiped out/occupied. A "Big Thanks!" to Scrabblette for watching Zuperfliegen on several occasions (and posting fun pictures on Facebook) - and to the several others who volunteered, but didn't get the chance! (Popular boy, that Zuperfliegen.)
[UPDATE THAT I ADDED LATER: The day after I posted this, I got some good news. See my next post for the details!]
OK, the rest of this post is going to talk about my penis. I've learned from previous posts that some of my Gentler Readers may think it's inappropriate for me to write, or at least for them to read, such things. If that sounds like you, then you should stop reading NOW.
No, seriously, if you think you might be offended or disturbed, then "Thank You!" for reading to here, but please stop NOW!
So, pretty wimpy of those other readers, eh? Mostly just kidding; I think in most cases people shouldn't read things that disturb them. But it seems silly to talk about removal of one's prostrate without talking about the penis. It's not the loss of the prostate itself that is the issue; it's the effects on the rest of the body.
- The urethra passes through the prostate. So my urethra had to be cut and then reattached. While that heals, I have a catheter (tube) running through my urethra from the bladder through the penis to an urine bag strapped to my leg. In a way, it's convenient, in that it avoids any incontinence. But, mostly, the idea, sight and feel of it is unsettling and, like just about every man who's had this operation, I'm very much looking forward to tomorrow (15 December), when it will most likely be taken out and I can return to normal-ish.
- Of course, the next question is "What's my new normal?". That is, once the catheter is removed, I get to find out how much incontinence is a problem. I'm hopeful, because I've been doing my pelvic floor exercies for months, that the problems will not be severe and that they will be short-lived. But I suspect that there will be an adjustment period, at the least, and I'll be using pads for a few weeks now. They're basically the same as "sanitary pads" for women, with slight modification for men's anatomy. Workable, but not the most comfortable or dignified things to wear. (sigh)
- Once I get started on that, I then have to start looking at getting my erections back. With the nerve-sparing surgery, I should have an excellent chance of that happening in 6-12 months (or maybe a little longer). The issue is that the nerves surrounding the prostate are the ones that signal the body to send blood to the penis to create the erection. Those nerves are currently in a state of shock (metaphorically) and need those months to recover. In the meantime, I need to produce erections through other means to keep the spongy tissues from scarring through disuse. So the plan is to use Viagra, or some similar drug or some other treatment that produces erections, to periodically keep the system active while the nerves work out the re-wiring of their purpose.
Hey, thanks very much for reading so very much about my somewhat humble life and my thoughts and feelings about it! I hope that something here has been useful or entertaining or otherwise meaningful for you.
So far, it is going well, in that I am able to get around on my own - albeit slowly and carefully - and there is almost no pain (just some discomfort from having an incision across my abdomen). Every day I have felt a little bit better and I remain basically hopeful and optimistic about the future. I hope that I am now "cured" of my prostate cancer - because we have removed it all from my body - but will probably not know anything more definitive until my follow-up appointment with the surgeon/urologist in about six weeks. The story goes on...(as always).
It has taken me three days of being back at home to finally get this blog entry written. That's partly because I have been focusing strongly on just relaxing/recovering and keeping up with my medications and post-operation procedures, and partly because, as you already know, it takes me a long time to actually get anything composed/written (sigh). As usual, my apologies for the delay (if you were waiting for a post-surgery update).
So that's pretty much the main news. The rest of this post is Other Notes about my time in the hopsital, my condition, and possibilities for the future:
- On 8 December, Ann and I arrived at the hospital for my admission at 6:30 AM, as instructed. (Many thanks to Tee for getting up so early and watching Zuperfliegen so that Ann could attend!) I was taken into surgery at 12:30 PM! It turns out they have all the morning surgery patients come in at the same time - so they have flexibility if they need to shuffle the schedule - and I was apparently pretty close to the bottom of the list. So the most effective method for the hospital was for me to get up early and sit around for six hours? Perhaps this is a function of being treated in the "public" health system.
- Ann and I had been told that the surgery would be 2-3 hours in duration. But I came out of the anaesthetic around 6:00 PM, suggesting that it may have actually lasted about 5 hours! I don't begrudge the medical personnel this difference; I wanted them to be able to do whatever they needed, no matter how long it took. Still, it was a little odd, and it made Ann anxious that no updates were coming when she expected them.
- I got to see my surgeon/urologist shortly before being taken into the operating theatre. He was the first one I saw when I was initially referred to a specialist for my suspicious PSA levels. At the time of my surgery, I had not seen him for a couple of months or more. I asked him about the difference in the plan for my lymph nodes. Specifically: When I first saw him as a private patient, his plan was to remove my lymph nodes (for further analysis of whether the cancer had spread past the prostate), as well as do a nerve-sparing surgery. But when I thought I might have a "robotic" surgery done, I was referred to his collegaue, who thought my lymph nodes should not be removed, and I should not have a nerve-sparing surgery. The fact that the two experts held diametrically opposed views on these issues was unsettling! Then, when I balked at the potential cost of private surgery, they referred me to the clinical trial and I was randomly assigned to the first/original urologist and told that my lymph nodes would not be removed, but he would do the nerve-sparing surgery. So when I asked him about this before the surgery, he said the clinical trial has protocols it has to follow; and that there was probably a 2% chance that cancer had spread to the lymph nodes, but possibly a greater percentage of there being unwanted complications if we removed them. It all sounded to me a little like "we give you the answer that best matches the current version of the situation". Which is potentially problematic, but it does underscore the uncertainties that exist with cancer and surgery in general. And, ultimately, as the patient, you have to do the best research you can so you can make the best decision you can; and then it still comes down to putting yourself in the care of the surgeon and hoping/assuming/believing that he or she will do the best they can and that will be enough.
- The surgeon also casually mentioned that I might need radiotherapy treatments later, because of the nerve-sparing surgery. um...WHAT? The idea is that the nerves being spared are wrapped around the prostate; so the surgeon leaves the outer layer of the prostate such that the nerves still have tissue to cling to and are not irreparably damaged. But if the remaining tissue has cancer cells, then I've still got a problem. This is what "positive margins" means in the analysis of my removed prostate. If the outer edge (margin) of the removed prostate is positive for cancer cells, then it is likely they are also still in the unremoved tissue and further treatment - radiation therapy, in this case - is called for. I knew all of this from my original consultation, I guess; but the emphasis for months has been on "we remove the prostate and cure the cancer!" and it was a little weird to be told/reminded that I may have to go through another involved/invasive procedure at some point in the future. Oh well, like I said: the story goes ever on...
- Coming out of the anesthetic and then getting an occasional self-administered dose of morphine made the first evening/night a bit weird. I believe I was reasonably aware and I think I remember pretty much everything, but I just couldn't keep my eyes open. I was not thrilled with the woozy, out-of-control experience. Once I realized that the morphine contributed to that, I decided to totally stop using it. (I didn't really need it, as the discomfort was minimal.). When I woke up the next morning (9 December), I thought, "Ah, now I'm really awake!"
- On 9 December (the day after my surgery), the registrar (essentially co-surgeon or assistant surgeon) for my operation stopped by and said that everything went swimmingly. I think that's probably true, but I also thought "Well, of course you're going to say that...". She also said that I would probably be discharged the next morning.
- However, despite 9 December being a pretty good recovery day (in that I was able to get out of bed and walk), on the morning of 10 December my blood pressure dropped low again and I got a bit dizzy when I tried to stand. My blood pressure is typically lowish, but it dropped down even lower than usual. So the doctors decided to keep me for another day for observation. That was disappointing and frustrating, as I was planning to go home. However, in hindsight, it was probably for the best. That was not a very good day, though, with me just able to lie in my bed.
- 11 December was much better. I slept well the night before, I felt much better in the morning, my blood pressure returned to normal-ish, and I was able to walk well enough. So I got to go home!
- In typing the above, it sounds like I had a lot to complain about. That's not really true, though. The above points are just some of the key items I had to think about. In general, I was pretty impressed with the professionalism and competence of the many medical professionals that attended to me. It's just that recovery in general, and hospital stays in particular (when you are, after all, the most unwell) are not typically fun experiences.
- It was great having Ann, and often Zuperfliegen, come visit me, of course. It's probably just as well there weren't other visitors, though, as it was a shortish hospital stay and I was somewhat wiped out/occupied. A "Big Thanks!" to Scrabblette for watching Zuperfliegen on several occasions (and posting fun pictures on Facebook) - and to the several others who volunteered, but didn't get the chance! (Popular boy, that Zuperfliegen.)
[UPDATE THAT I ADDED LATER: The day after I posted this, I got some good news. See my next post for the details!]
OK, the rest of this post is going to talk about my penis. I've learned from previous posts that some of my Gentler Readers may think it's inappropriate for me to write, or at least for them to read, such things. If that sounds like you, then you should stop reading NOW.
No, seriously, if you think you might be offended or disturbed, then "Thank You!" for reading to here, but please stop NOW!
So, pretty wimpy of those other readers, eh? Mostly just kidding; I think in most cases people shouldn't read things that disturb them. But it seems silly to talk about removal of one's prostrate without talking about the penis. It's not the loss of the prostate itself that is the issue; it's the effects on the rest of the body.
- The urethra passes through the prostate. So my urethra had to be cut and then reattached. While that heals, I have a catheter (tube) running through my urethra from the bladder through the penis to an urine bag strapped to my leg. In a way, it's convenient, in that it avoids any incontinence. But, mostly, the idea, sight and feel of it is unsettling and, like just about every man who's had this operation, I'm very much looking forward to tomorrow (15 December), when it will most likely be taken out and I can return to normal-ish.
- Of course, the next question is "What's my new normal?". That is, once the catheter is removed, I get to find out how much incontinence is a problem. I'm hopeful, because I've been doing my pelvic floor exercies for months, that the problems will not be severe and that they will be short-lived. But I suspect that there will be an adjustment period, at the least, and I'll be using pads for a few weeks now. They're basically the same as "sanitary pads" for women, with slight modification for men's anatomy. Workable, but not the most comfortable or dignified things to wear. (sigh)
- Once I get started on that, I then have to start looking at getting my erections back. With the nerve-sparing surgery, I should have an excellent chance of that happening in 6-12 months (or maybe a little longer). The issue is that the nerves surrounding the prostate are the ones that signal the body to send blood to the penis to create the erection. Those nerves are currently in a state of shock (metaphorically) and need those months to recover. In the meantime, I need to produce erections through other means to keep the spongy tissues from scarring through disuse. So the plan is to use Viagra, or some similar drug or some other treatment that produces erections, to periodically keep the system active while the nerves work out the re-wiring of their purpose.
Hey, thanks very much for reading so very much about my somewhat humble life and my thoughts and feelings about it! I hope that something here has been useful or entertaining or otherwise meaningful for you.
Tuesday 8 November 2011
My Cancer: How It All Began, or, 'To PSA Or Not To PSA?'
When I first posted news about my prostate cancer (here, with the later update here), several people asked how I found out about it. It's odd that I didn't include that in my original post; but I'm going to rectify that now.
In December 2010, I went to a general practitioner for a small, totally unrelated medical matter. As part of the general check-up, he thought I should have some blood tests done, as well as a digital rectal exam (known everywhere to men as the "finger up the butt" exam). Due to my age - 47 at the time - I was more at risk for prostate cancer and/or, more likely, benign prostatic hyperplasia (BPH), an enlargement of the prostate that can lead to urinary difficulties. According to Wikipedia, "Adenomatous prostatic growth is believed to begin at approximately age 30 years. An estimated 50% of men have histologic evidence of BPH by age 50 years and 75% by age 80 years. In 40-50% of these patients, BPH becomes clinically significant."
The digital rectal exam revealed nothing unusual; but the blood tests revealed elevated PSA levels. PSA stands for prostate-specific antigen, a protein produced by the normal function of the prostate. In the case of prostate cancer, PSA levels in the blood may rise above normal levels. However, non-cancerous events, like having sex or riding a bike, can also lead to temporarily elevated PSA levels.
My PSA value was 4.1, when the recommended level is less than 2.5. My general practitioner referred me to an urologist (the same one that will be doing my surgery on 8 December). He repeated the digital rectal exam with the same results (nothing), and then recommended I take anti-inflammatory drugs for a couple of weeks and repeat the PSA blood screen in February 2011.
MY PSA level was 2.7 in February. Definitely lower, but still not quite where we would like it. We decided to look at it again in a couple of months.
In April, the level was 3.3. The urologist recommended we do a biopsy. I was hesitant, as that involved an invasive procedure. So we decided to wait a few more months.
In July my PSA level was 2.7 again. The doctor said that was about twice what it should be and, while it was not going up, it also was not going down. He again suggested the biopsy and I agreed. That was conducted later that month and, as I reported earlier, 14 of the 16 samples taken contained cancer.
This history is interesting to me in light of recent developments in the healthcare arena. The United States Preventive Services Task Force recently recommended that doctors no longer use the PSA test to screen for prostate cancer. (You can read about it here and here.) Also, a book was recently released that takes the position that most men with prostate cancer should not seek surgery or radiation treatments.
I understand the perspectives presented by those sources, and I'm even a bit sympathetic to them. However, I still believe that surgery is definitely the best option for my situation. Prostate cancer tends to grow/spread slowly. So, for many men, something else will kill them before the cancer does. However, I'm not even 50 yet and I plan to spend quite a few more years alive. I figure the longer I wait, the more likely it is that the cancer metastasizes and I'm in serious trouble. I'm not willing to bet that the cancer will not spread in the next 20 years. Even 10 years would seem like a risky bet to me.
If that makes sense, then it follows that the PSA test was a good thing for me. Without it, I probably never would have known I had cancer until it spread and affected some other organ.
I'm just one case, though. It's entirely possible that the vast majority of men who are tested and found to have elevated PSA levels are better off not knowing and not seeking treatment. If so, that's a lot of unnecessary treatments and post-treatment difficulties. The statistics from one of the studies suggest that 47 out of 48 men fall into that category. So I can see why the panel would recommend not using the test. But for that one guy (and his family and friends), it's a very different story!
Unfortunately, life doesn't come with a control group; so we'll never know what would happen if I don't have the surgery. "You roll the dice and you take the chance."
I did ask my second urologist (the robotic surgery expert) about the no-PSA recommendation. He believes that U.S. doctors tend to over-treat prostate cancer, rushing to surgery or radiation when a wait-and-see approach may be more reasonable.
Ultimately, I come down on the same side I always do: knowledge. Or, as I like to say: "knowledge over sanity". I think it's good to know things, including how some of the things you "know" can be wrong or misleading. So I support the PSA test, but think that conclusions have to be reached in context, and that it's useful to not blindly accept what a doctor tells you (though it's hard not to, given the average person's ignorance about these issues; I include myself in that category!). It wasn't the PSA result that led me to choose surgery. It was the trend of multiple PSA results that led me to the biopsy, and it was the biopsy results - interpreted in the context of my age, overall health, etc. - that has led to the surgery.
In December 2010, I went to a general practitioner for a small, totally unrelated medical matter. As part of the general check-up, he thought I should have some blood tests done, as well as a digital rectal exam (known everywhere to men as the "finger up the butt" exam). Due to my age - 47 at the time - I was more at risk for prostate cancer and/or, more likely, benign prostatic hyperplasia (BPH), an enlargement of the prostate that can lead to urinary difficulties. According to Wikipedia, "Adenomatous prostatic growth is believed to begin at approximately age 30 years. An estimated 50% of men have histologic evidence of BPH by age 50 years and 75% by age 80 years. In 40-50% of these patients, BPH becomes clinically significant."
The digital rectal exam revealed nothing unusual; but the blood tests revealed elevated PSA levels. PSA stands for prostate-specific antigen, a protein produced by the normal function of the prostate. In the case of prostate cancer, PSA levels in the blood may rise above normal levels. However, non-cancerous events, like having sex or riding a bike, can also lead to temporarily elevated PSA levels.
My PSA value was 4.1, when the recommended level is less than 2.5. My general practitioner referred me to an urologist (the same one that will be doing my surgery on 8 December). He repeated the digital rectal exam with the same results (nothing), and then recommended I take anti-inflammatory drugs for a couple of weeks and repeat the PSA blood screen in February 2011.
MY PSA level was 2.7 in February. Definitely lower, but still not quite where we would like it. We decided to look at it again in a couple of months.
In April, the level was 3.3. The urologist recommended we do a biopsy. I was hesitant, as that involved an invasive procedure. So we decided to wait a few more months.
In July my PSA level was 2.7 again. The doctor said that was about twice what it should be and, while it was not going up, it also was not going down. He again suggested the biopsy and I agreed. That was conducted later that month and, as I reported earlier, 14 of the 16 samples taken contained cancer.
This history is interesting to me in light of recent developments in the healthcare arena. The United States Preventive Services Task Force recently recommended that doctors no longer use the PSA test to screen for prostate cancer. (You can read about it here and here.) Also, a book was recently released that takes the position that most men with prostate cancer should not seek surgery or radiation treatments.
I understand the perspectives presented by those sources, and I'm even a bit sympathetic to them. However, I still believe that surgery is definitely the best option for my situation. Prostate cancer tends to grow/spread slowly. So, for many men, something else will kill them before the cancer does. However, I'm not even 50 yet and I plan to spend quite a few more years alive. I figure the longer I wait, the more likely it is that the cancer metastasizes and I'm in serious trouble. I'm not willing to bet that the cancer will not spread in the next 20 years. Even 10 years would seem like a risky bet to me.
If that makes sense, then it follows that the PSA test was a good thing for me. Without it, I probably never would have known I had cancer until it spread and affected some other organ.
I'm just one case, though. It's entirely possible that the vast majority of men who are tested and found to have elevated PSA levels are better off not knowing and not seeking treatment. If so, that's a lot of unnecessary treatments and post-treatment difficulties. The statistics from one of the studies suggest that 47 out of 48 men fall into that category. So I can see why the panel would recommend not using the test. But for that one guy (and his family and friends), it's a very different story!
Unfortunately, life doesn't come with a control group; so we'll never know what would happen if I don't have the surgery. "You roll the dice and you take the chance."
I did ask my second urologist (the robotic surgery expert) about the no-PSA recommendation. He believes that U.S. doctors tend to over-treat prostate cancer, rushing to surgery or radiation when a wait-and-see approach may be more reasonable.
Ultimately, I come down on the same side I always do: knowledge. Or, as I like to say: "knowledge over sanity". I think it's good to know things, including how some of the things you "know" can be wrong or misleading. So I support the PSA test, but think that conclusions have to be reached in context, and that it's useful to not blindly accept what a doctor tells you (though it's hard not to, given the average person's ignorance about these issues; I include myself in that category!). It wasn't the PSA result that led me to choose surgery. It was the trend of multiple PSA results that led me to the biopsy, and it was the biopsy results - interpreted in the context of my age, overall health, etc. - that has led to the surgery.
Sunday 30 October 2011
A Cancer Update: My Surgery Is Scheduled For December 8
My original post about my prostate cancer was written on August 14. At that time, it looked like I would have an appointment with my urologist in September and we would make the final decisions about the treatment and probably schedule the surgery for the first week in October. Well, things didn't turn out that way and now my surgery is "definitely" scheduled for December 8.
Here's what happened:
On the appointment date in September, I got an MRI done so the results would be available when I saw my urologist. It's supposed to give a better picture of whether the cancer has spread beyond the prostate. The good news is that it didn't show any spreading. Of course, my urologist did point out there's always the possibility that it has already spread in microscopic pieces too small for the MRI to pick up. Thanks a lot, Mr. Upbeat Health Professional! Still, it does underscore the fact that all forms of treatment (and even non-treatment) are just a roll of the dice, and we make the best decisions we can based on the probabilities as we understand them.
Radical prostatectomy surgery (removal of the prostate) was still deemed the most effective choice for dealing with - curing, actually - the cancer. I just needed to decide if I wanted to go with "open" (traditional) surgery or "robot"(-assisted) surgery. Robot surgery is less intrusive, leaves less of a scar and allows for faster initial recovery, so I would be able to leave the hospital 2-3 days earlier. However, it also costs $3,000 more, and none of that would be covered by Medicare or my private health insurance. Based on the idea that the cost of the general surgery would be nominal (from my experience with knee surgery a few years ago), I (in consultation with Ann) decided to go with the robotic option. That, however, meant that the surgery would be done by another urologist, a colleague of my original doctor, who has done more robotic surgeries than anyone in Australia. So we set up an appointment with him, which was scheduled for one or two weeks later.
I also got a hint that the surgery was going to cost more than I originally thought. So during the time before my next appointment, I made some inquiries about exact costs and discovered that I (and Ann) would end up paying $9-10,000 "out-of-pocket" (the amount that would not be covered by Medicare or private insurance). This was shocking to us, as it represented about 6 months of us aggressively saving.
Yes, I know that some of you are thinking "$10,000 is nothing compared to the extension of one's life and the avoidance of active cancer." And, you're (mostly) right. But where do you draw the line? Would you pay $20,000? 50,000? $100,000? Would you sell yourself out as someone's slave (or indentured servant) for a year? For the rest of your life? So if the line is going to be drawn somewhere, is it that odd to think it should be drawn at less than $10,000? Especially if one lives in a country, like Australia, with a public health system in which you can get the surgery done for FREE. (Or, rather, it is paid for through a collective organisation funded by one's own, and other citizens', taxes.)
You see, I had been unknowingly moved to the world of private healthcare (as opposed to the public health system) by following my general practitioner's referral without thinking about it too much (combined with the ignorance of an immigrant - that's me! - about the difference between the two systems). So I took it upon myself to learn more about how all this worked.
I am a little dismayed, though, that I got to the point of scheduling my surgery before there was discussion of what it was all going to cost me. Clearly, I should have been asking more questions earlier. Still, I think the whole process should be like many of the restaurants in Australia - which include a copy of their menu outside the door so you can know in advance what the meal is going to cost and make an appropriate decision about eating there. (It would be great if more American restaurants did the same thing...)
Anyway, so my appointment with the robotic surgeon/urologist mostly involved me asking "how do we get this moved to the public system and what effect will that have on the treatment?" One important point was that the robotic surgery was not available in the public system. After hearing my concerns, he thought that going public would be a good option for me. And, he offered to refer me to a clinical trial that was being run by him and the other urologist/surgeon (and the University of Queensland and the Australian Cancer Council). It's comparing the effectiveness of robotic vs. open surgery for radical prostatectomy. Once in the study, I would be randomly assigned to one of the treatment options; so there would still be a chance to have the robotic surgery. Open surgery would be done by my original urologist, and robotic surgery would be done by the other doctor - both essentially at the top of their fields in Australia.
To make a long story short (oh, wait, too late!), I said "yes, please, sign me up!" I was given very little information about when things would happen, but was told I might have to wait 4-6 months for the surgery. That concerned me, since the whole idea is to cut out the cancer before it can spread from the prostate. I took solace from the fact that prostate cancer tends to be very slow-growing. Ultimately, though, I went through the bureaucratic phone tag at the hospital that is running the study and managed to connect with the coordinator of the clinical trial. She was very helpful and provided me with all the information I needed. She also got me scheduled for an intake appointment, where I was officially added to the trial and "randomised". It turns out I will be having the open surgery with my original urologist. I'm a little bummed that I was unable to get the less-invasive robotic surgery, but I have a great deal of faith and respect for the experience and skills of the surgeon who will be performing the operation. And, of course, Ann and I are happy that we have "saved" $9-10,000. Hooray for socialised medicine!
I have been scheduled for a "pre-admission clinic" on November 24 (Thanksgiving in the USA!), where I will spend several hours in the hospital meeting the professionals who will be involved in my operation, as well as having various tests done and analysed. Then, I will go in for my surgery on December 8 (the 70th anniversary of the USA declaring war on Japan in World War II - the day after the "date that will live in infamy"). I will then be in the hospital for 3-5 days, after which I will be at home recovering for six weeks. It should make for a mild Christmas season....
A summary of how I'm feeling about all of this these days:
I'm happy that everything has been organised. I'm thrilled that the Australian public health system is continuing to impress me. I'm looking forward to (probably) being cancer-free and eventually partaking in the future adventures life has in store for me.
I'm a bit anxious about the possible after-effects of the surgery - see my previous post for details - and disturbed by not knowing how severe, or not, they will be. There's probably a little depression, but I honestly don't think it's having much of an impact on my day-to-day life. I still laugh when I talk about my cancer. I'm still fatalistically hopeful...or, perhaps, hopefully fatalistic.
I look at the probability ambiguity as "it's always possible to lose," but I still hope (and try to plan) for the best. We'll know the result in the end, and it will be what it will be. I figure that if I die in the next 10 years - from cancer or being hit by a bus or anything else - the surgery will have been a "mistake" (but I'll be dead, so I'll never know or care). And if I live longer than 10 more years, I think I will have made the right decision.
More news as it comes about, which will probably be after December 8. However, I'm planning to compose another blog entry shortly after this one that talks about how I found out I have cancer and my thoughts on the ongoing PSA debate. [UPDATE: It has been written and can be seen here.]
Here's what happened:
On the appointment date in September, I got an MRI done so the results would be available when I saw my urologist. It's supposed to give a better picture of whether the cancer has spread beyond the prostate. The good news is that it didn't show any spreading. Of course, my urologist did point out there's always the possibility that it has already spread in microscopic pieces too small for the MRI to pick up. Thanks a lot, Mr. Upbeat Health Professional! Still, it does underscore the fact that all forms of treatment (and even non-treatment) are just a roll of the dice, and we make the best decisions we can based on the probabilities as we understand them.
Radical prostatectomy surgery (removal of the prostate) was still deemed the most effective choice for dealing with - curing, actually - the cancer. I just needed to decide if I wanted to go with "open" (traditional) surgery or "robot"(-assisted) surgery. Robot surgery is less intrusive, leaves less of a scar and allows for faster initial recovery, so I would be able to leave the hospital 2-3 days earlier. However, it also costs $3,000 more, and none of that would be covered by Medicare or my private health insurance. Based on the idea that the cost of the general surgery would be nominal (from my experience with knee surgery a few years ago), I (in consultation with Ann) decided to go with the robotic option. That, however, meant that the surgery would be done by another urologist, a colleague of my original doctor, who has done more robotic surgeries than anyone in Australia. So we set up an appointment with him, which was scheduled for one or two weeks later.
I also got a hint that the surgery was going to cost more than I originally thought. So during the time before my next appointment, I made some inquiries about exact costs and discovered that I (and Ann) would end up paying $9-10,000 "out-of-pocket" (the amount that would not be covered by Medicare or private insurance). This was shocking to us, as it represented about 6 months of us aggressively saving.
Yes, I know that some of you are thinking "$10,000 is nothing compared to the extension of one's life and the avoidance of active cancer." And, you're (mostly) right. But where do you draw the line? Would you pay $20,000? 50,000? $100,000? Would you sell yourself out as someone's slave (or indentured servant) for a year? For the rest of your life? So if the line is going to be drawn somewhere, is it that odd to think it should be drawn at less than $10,000? Especially if one lives in a country, like Australia, with a public health system in which you can get the surgery done for FREE. (Or, rather, it is paid for through a collective organisation funded by one's own, and other citizens', taxes.)
You see, I had been unknowingly moved to the world of private healthcare (as opposed to the public health system) by following my general practitioner's referral without thinking about it too much (combined with the ignorance of an immigrant - that's me! - about the difference between the two systems). So I took it upon myself to learn more about how all this worked.
I am a little dismayed, though, that I got to the point of scheduling my surgery before there was discussion of what it was all going to cost me. Clearly, I should have been asking more questions earlier. Still, I think the whole process should be like many of the restaurants in Australia - which include a copy of their menu outside the door so you can know in advance what the meal is going to cost and make an appropriate decision about eating there. (It would be great if more American restaurants did the same thing...)
Anyway, so my appointment with the robotic surgeon/urologist mostly involved me asking "how do we get this moved to the public system and what effect will that have on the treatment?" One important point was that the robotic surgery was not available in the public system. After hearing my concerns, he thought that going public would be a good option for me. And, he offered to refer me to a clinical trial that was being run by him and the other urologist/surgeon (and the University of Queensland and the Australian Cancer Council). It's comparing the effectiveness of robotic vs. open surgery for radical prostatectomy. Once in the study, I would be randomly assigned to one of the treatment options; so there would still be a chance to have the robotic surgery. Open surgery would be done by my original urologist, and robotic surgery would be done by the other doctor - both essentially at the top of their fields in Australia.
To make a long story short (oh, wait, too late!), I said "yes, please, sign me up!" I was given very little information about when things would happen, but was told I might have to wait 4-6 months for the surgery. That concerned me, since the whole idea is to cut out the cancer before it can spread from the prostate. I took solace from the fact that prostate cancer tends to be very slow-growing. Ultimately, though, I went through the bureaucratic phone tag at the hospital that is running the study and managed to connect with the coordinator of the clinical trial. She was very helpful and provided me with all the information I needed. She also got me scheduled for an intake appointment, where I was officially added to the trial and "randomised". It turns out I will be having the open surgery with my original urologist. I'm a little bummed that I was unable to get the less-invasive robotic surgery, but I have a great deal of faith and respect for the experience and skills of the surgeon who will be performing the operation. And, of course, Ann and I are happy that we have "saved" $9-10,000. Hooray for socialised medicine!
I have been scheduled for a "pre-admission clinic" on November 24 (Thanksgiving in the USA!), where I will spend several hours in the hospital meeting the professionals who will be involved in my operation, as well as having various tests done and analysed. Then, I will go in for my surgery on December 8 (the 70th anniversary of the USA declaring war on Japan in World War II - the day after the "date that will live in infamy"). I will then be in the hospital for 3-5 days, after which I will be at home recovering for six weeks. It should make for a mild Christmas season....
A summary of how I'm feeling about all of this these days:
I'm happy that everything has been organised. I'm thrilled that the Australian public health system is continuing to impress me. I'm looking forward to (probably) being cancer-free and eventually partaking in the future adventures life has in store for me.
I'm a bit anxious about the possible after-effects of the surgery - see my previous post for details - and disturbed by not knowing how severe, or not, they will be. There's probably a little depression, but I honestly don't think it's having much of an impact on my day-to-day life. I still laugh when I talk about my cancer. I'm still fatalistically hopeful...or, perhaps, hopefully fatalistic.
I look at the probability ambiguity as "it's always possible to lose," but I still hope (and try to plan) for the best. We'll know the result in the end, and it will be what it will be. I figure that if I die in the next 10 years - from cancer or being hit by a bus or anything else - the surgery will have been a "mistake" (but I'll be dead, so I'll never know or care). And if I live longer than 10 more years, I think I will have made the right decision.
More news as it comes about, which will probably be after December 8. However, I'm planning to compose another blog entry shortly after this one that talks about how I found out I have cancer and my thoughts on the ongoing PSA debate. [UPDATE: It has been written and can be seen here.]
Monday 17 October 2011
A Zuperfliegen Update: Sehr fliegen für einen weißen Mann
Zupe recently celebrated his six-month birthday! Kind of amazing to think that we are already halfway through his first year.
The BIG news, though, is that he is off the oxygen! We took him in for his second sleep study last month. (His first sleep study was shortly after he was born and was the determinant for him being placed on oxygen.) He breathed just fine and the doctors said we could take him off the oxygen. We were floored, because we had originally been told that he would likely be on oxygen for a year and that only one child had ever been taken off after three months, and even then they were dubious about it. When we asked about that after last month's decision, the doctor said "I don't know why you were told that; we take children off after three months all the time." I guess the first nurse was just helping us adjust our expectations.
So that's pretty cool. Having him on oxygen was annoying, but totally manageable. We just had to make sure that we always had a tank with us, and that we chose the best route for the tubing to follow when we walked around the house. So we could still do all the things "normal" babies and parents were doing, we just had to think/plan a little more. Still, it was real relief to hear we didn't have to do that any longer. Most of the relief was, undoubtedly, just knowing that our son was finally breathing well on his own!
The other developmental advance is that we have heard Zuperfliegen laugh! It happened several weeks ago when we were just playing around with him. What a delight that was! Shortly after, Ann was able to catch his laugh on video, which you can see here - there are other videos of him there, too. The funny thing is, he didn't laugh again for weeks and weeks! I guess Ann and I are not as funny as we thought; or, his taste in comedy is just so much more refined than our own! The "drought" did end this evening, when Ann got him to laugh again. We also think he has his own special short laugh, which is kind of like that of the Sheldon character on The Big Bang Theory.
In general, he's doing really well. He's eating and growing like a champ without getting fat (we think), he's generally very mild and well-behaved, and his eczema has cleared up tremendously with the application of steroidal cream (which we're hoping to eventually no longer need).
We're still a little concerned about the development of his gross motor skills, particularly with regards to being on his stomach (he's still not a fan of "tummy time") and his ability to roll over (which he has yet to do, though he's getting closer). We're mostly feeling that he is just going at his own pace and we're letting him step to the beat of his different drummer. But we also have a couple of appointments with physiotherapists to get some more opinions.
As for me, I continue with my revelation of "wow, this experience of being a father and having a child in one's life is pretty cool!" It all sounds pretty simple - and perhaps banal - but anyone who knew me in the first 40 years of my life should be shocked. I am very aware, though, that a big part of me finding the experience pleasant has to do with Ann both being a such a great mother and taking a huge share of the childcare responsibilities. Fortunately, she's really digging the experience, too.
I also want to remind you that more about Ann's perspective can be found at her blog: http://nnv-a-blog-downunder.blogspot.com. She also posts a LOT more pictures than I do - with even more at her photography blog: http://nnv-inmyeye.blogspot.com
[Update on 24 October 2011]: Zupe went to his appointments with two different physiotherapists - one in the private healthcare system and one in the public healthcare system. Both said he was doing fine and they were generally unconcerned about his development. At the same time, they showed Ann a variety of exercises we could have him do to aid proper, balanced development. Meanwhile, he's also "talking" an awful lot. It's mainly various guttural grunts and the like, be he really goes on for a while sometimes! We're pretty pleased with all this!
The BIG news, though, is that he is off the oxygen! We took him in for his second sleep study last month. (His first sleep study was shortly after he was born and was the determinant for him being placed on oxygen.) He breathed just fine and the doctors said we could take him off the oxygen. We were floored, because we had originally been told that he would likely be on oxygen for a year and that only one child had ever been taken off after three months, and even then they were dubious about it. When we asked about that after last month's decision, the doctor said "I don't know why you were told that; we take children off after three months all the time." I guess the first nurse was just helping us adjust our expectations.
So that's pretty cool. Having him on oxygen was annoying, but totally manageable. We just had to make sure that we always had a tank with us, and that we chose the best route for the tubing to follow when we walked around the house. So we could still do all the things "normal" babies and parents were doing, we just had to think/plan a little more. Still, it was real relief to hear we didn't have to do that any longer. Most of the relief was, undoubtedly, just knowing that our son was finally breathing well on his own!
The other developmental advance is that we have heard Zuperfliegen laugh! It happened several weeks ago when we were just playing around with him. What a delight that was! Shortly after, Ann was able to catch his laugh on video, which you can see here - there are other videos of him there, too. The funny thing is, he didn't laugh again for weeks and weeks! I guess Ann and I are not as funny as we thought; or, his taste in comedy is just so much more refined than our own! The "drought" did end this evening, when Ann got him to laugh again. We also think he has his own special short laugh, which is kind of like that of the Sheldon character on The Big Bang Theory.
In general, he's doing really well. He's eating and growing like a champ without getting fat (we think), he's generally very mild and well-behaved, and his eczema has cleared up tremendously with the application of steroidal cream (which we're hoping to eventually no longer need).
We're still a little concerned about the development of his gross motor skills, particularly with regards to being on his stomach (he's still not a fan of "tummy time") and his ability to roll over (which he has yet to do, though he's getting closer). We're mostly feeling that he is just going at his own pace and we're letting him step to the beat of his different drummer. But we also have a couple of appointments with physiotherapists to get some more opinions.
As for me, I continue with my revelation of "wow, this experience of being a father and having a child in one's life is pretty cool!" It all sounds pretty simple - and perhaps banal - but anyone who knew me in the first 40 years of my life should be shocked. I am very aware, though, that a big part of me finding the experience pleasant has to do with Ann both being a such a great mother and taking a huge share of the childcare responsibilities. Fortunately, she's really digging the experience, too.
I also want to remind you that more about Ann's perspective can be found at her blog: http://nnv-a-blog-downunder.blogspot.com. She also posts a LOT more pictures than I do - with even more at her photography blog: http://nnv-inmyeye.blogspot.com
[Update on 24 October 2011]: Zupe went to his appointments with two different physiotherapists - one in the private healthcare system and one in the public healthcare system. Both said he was doing fine and they were generally unconcerned about his development. At the same time, they showed Ann a variety of exercises we could have him do to aid proper, balanced development. Meanwhile, he's also "talking" an awful lot. It's mainly various guttural grunts and the like, be he really goes on for a while sometimes! We're pretty pleased with all this!
Sunday 14 August 2011
Is Kevin Dying Of Cancer?
Possibly. (But probably not.)
I have been diagnosed with prostate cancer. A lot of it, actually. When they did a biopsy of my prostate, they took samples from 16 different areas of the organ. 14 of them had cancer cells!
(The prostate surrounds part of the urethra between the bladder and the penis. Its function is to store and secrete a fluid that comprises 20-30% of the seminal discharge upon ejaculation.)
But it is not as bad as it sounds. Really. My urologist thinks it is highly likely that the cancer is entirely contained to my prostate; that is, it has not spread to the surrounding organs or entered my bloodstream or lymph channels. This means that if we remove the prostate - and that looks like what will happen - the cancer will be removed from my body. I will be completely cured. (Of course, I will have to be medically vigilant for the rest of my life to verify that remains the case. But that will just be periodic blood tests and maybe bone scans.)
You see, in the minds of most people, Cancer = Death (and it is bolded just like that in their minds, too). But that is often not the case, and I am pretty sure that will be true for me, too. As I said, I expect to be completely cured of this cancer. So let's please not have any of those scenes where you have to look sad and say, "Oh, Kevin, I'm so sorry!" and I have to look sad and say, "Well, I'm trying to be strong..." I'm just not very good at looking sad. Remember, one of Kevin's Absolute Truths is "Life sucks, but is mostly worth living."
So, of course, there are real reasons for me to be annoyed and/or bummed out. The first is that I will have to have an operation and one of my organs will be removed. That will involve a hospital stay and weeks of recovery and some pain and hassle. More importantly, the surgical removal of my prostrate will have a 30-60% chance of leaving me with impotence/erectile dysfunction (the inability to get an erection) and a 5% chance of incontinence (inability to control urination). Even if I do not ultimately end up having those problems for the rest of my life, I will definitely have them for a period of time after the operation.
I think I would really miss my erections. They and I have had a lot of good times throughout my life. And, whether or not I end up impotent, I will no longer be able to ejaculate (wow, that will be weird) or reproduce (well, "normally", anyway; all the more reason to invest in cloning research!).
The idea of lifelong incontinence problems sounds like a real drag. I am glad that the odds are very much in my favour to avoid that and I sincerely hope it all works out.
But either or both of those problems would be preferable to being dead, or even experiencing the health complications that would accompany the cancer spreading. So the operation seems like a no-brainer to me. (With regards to other treatment options - radiotherapy, hormone therapy, cryotherapy, high frequency ultrasound, etc. - my urologist believes, and I concur, that because the cancer is so widespread in my prostate, it is likely that non-surgical treatments would not get all the cancer and I would have an unacceptable level of ongoing risk.)
OK, time for some good news!
My urologist has years of experience with treating prostate cancer and performing the surgery, and he is widely respected and seen as the "go to" guy for this by my general practitioner and some other doctors I know.
Also, I have accrued enough paid sick leave at my job to cover the time required for the surgery and recovery. More importantly, my boss is totally supportive of me doing what I need to do to take care of myself.
And Australia has an excellent Medicare-for-all system that keeps medical expenses within acceptable levels, which is further helped by the private health insurance I carry to cover hospitalisation expenses. So this should not break my and Ann's finances. (However, we do have a concern for how this "history of cancer" will affect my ability to get appropriate health insurance when we eventually move to the USA.)
Finally, one benefit of having cancer is that I can use it to get out of the difficult social situations in which I occasionally find myself. Because of my "unique" way of looking at the universe and human relations, I occasionally (inadvertently) rub some people the wrong way. When I detect that someone is thinking "Kevin is a jerk!" I should be able to get myself some slack by saying, "You know, I have cancer..." (Hmmm, it may work better if I look sad, though, and that might be problematic.)
I have been diagnosed with prostate cancer. A lot of it, actually. When they did a biopsy of my prostate, they took samples from 16 different areas of the organ. 14 of them had cancer cells!
(The prostate surrounds part of the urethra between the bladder and the penis. Its function is to store and secrete a fluid that comprises 20-30% of the seminal discharge upon ejaculation.)
But it is not as bad as it sounds. Really. My urologist thinks it is highly likely that the cancer is entirely contained to my prostate; that is, it has not spread to the surrounding organs or entered my bloodstream or lymph channels. This means that if we remove the prostate - and that looks like what will happen - the cancer will be removed from my body. I will be completely cured. (Of course, I will have to be medically vigilant for the rest of my life to verify that remains the case. But that will just be periodic blood tests and maybe bone scans.)
You see, in the minds of most people, Cancer = Death (and it is bolded just like that in their minds, too). But that is often not the case, and I am pretty sure that will be true for me, too. As I said, I expect to be completely cured of this cancer. So let's please not have any of those scenes where you have to look sad and say, "Oh, Kevin, I'm so sorry!" and I have to look sad and say, "Well, I'm trying to be strong..." I'm just not very good at looking sad. Remember, one of Kevin's Absolute Truths is "Life sucks, but is mostly worth living."
So, of course, there are real reasons for me to be annoyed and/or bummed out. The first is that I will have to have an operation and one of my organs will be removed. That will involve a hospital stay and weeks of recovery and some pain and hassle. More importantly, the surgical removal of my prostrate will have a 30-60% chance of leaving me with impotence/erectile dysfunction (the inability to get an erection) and a 5% chance of incontinence (inability to control urination). Even if I do not ultimately end up having those problems for the rest of my life, I will definitely have them for a period of time after the operation.
I think I would really miss my erections. They and I have had a lot of good times throughout my life. And, whether or not I end up impotent, I will no longer be able to ejaculate (wow, that will be weird) or reproduce (well, "normally", anyway; all the more reason to invest in cloning research!).
The idea of lifelong incontinence problems sounds like a real drag. I am glad that the odds are very much in my favour to avoid that and I sincerely hope it all works out.
But either or both of those problems would be preferable to being dead, or even experiencing the health complications that would accompany the cancer spreading. So the operation seems like a no-brainer to me. (With regards to other treatment options - radiotherapy, hormone therapy, cryotherapy, high frequency ultrasound, etc. - my urologist believes, and I concur, that because the cancer is so widespread in my prostate, it is likely that non-surgical treatments would not get all the cancer and I would have an unacceptable level of ongoing risk.)
OK, time for some good news!
My urologist has years of experience with treating prostate cancer and performing the surgery, and he is widely respected and seen as the "go to" guy for this by my general practitioner and some other doctors I know.
Also, I have accrued enough paid sick leave at my job to cover the time required for the surgery and recovery. More importantly, my boss is totally supportive of me doing what I need to do to take care of myself.
And Australia has an excellent Medicare-for-all system that keeps medical expenses within acceptable levels, which is further helped by the private health insurance I carry to cover hospitalisation expenses. So this should not break my and Ann's finances. (However, we do have a concern for how this "history of cancer" will affect my ability to get appropriate health insurance when we eventually move to the USA.)
Finally, one benefit of having cancer is that I can use it to get out of the difficult social situations in which I occasionally find myself. Because of my "unique" way of looking at the universe and human relations, I occasionally (inadvertently) rub some people the wrong way. When I detect that someone is thinking "Kevin is a jerk!" I should be able to get myself some slack by saying, "You know, I have cancer..." (Hmmm, it may work better if I look sad, though, and that might be problematic.)
Parenting Zuperfliegen: Four-Months-Plus In
Zuperfliegen recently turned four months old. Over the past couple of months, several friends have asked me how things were going. I have typically given a very short summary and added "I plan to write a more complete response soon". This blog entry is an attempt to finally do just that.
Let's first talk about Zuperfliegen's health. Overall, I think it is very good. He is eating and growing like a champ. His height and weight are both around the 70th percentile, with his head size a little higher than that (go, big-headed guys!). He is also sleeping through the night, as well as getting a few naps during the day. And today we saw what appears to be the start of his first tooth.
As you may remember, Zuperfliegen suffers from sleep apnea and requires oxygen 24 hours a day. This is a developmental issue and the prognosis is that he will develop out of it by the end of his first year. We are scheduled for a sleep study at the hospital every three months to monitor his progress and, eventually, determine when he can get off the oxygen. Our first sleep study was supposed to be on August 3. Unfortunately, Zupe had caught a cold at that time and the hospital did not want to do the study unless he was completely well. So the sleep study has been rescheduled for September 5. That was a little disappointing, as Ann and I were looking forward to hearing what progress he has made. But we recognise that it was highly unlikely that he was going to come off the oxygen at this point, so we can deal with waiting a little longer to hear about his current status. We do worry a little that this will push all the future sleep studies back a month, also.
Zuperfliegen has been suffering from an advanced case of eczema giving him a sandpaper-y feel to his skin. Ann has been pursuing various solutions, all with minimal effect. The current perspective, from Zupe's general practitioner, is that it is an allergic response triggered by the season (as it is winter here, the air is dry and cold). So she prescribed a standard moisturizer for babies, a strong steroidal topical cream, bath oil instead of soap, and the removal of gluten and dairy from the food Ann eats (as well as switching the formula for Zupe). We are hoping this, combined with the eventual change of season and warming of the days, will resolve the issue (and that we are eventually able to work gluten and dairy back into Ann's diet!).
The big news about Zuperfliegen is that we have been able to observe developmental changes:
(1) He is smiling! That has really made a big difference. Partly because it means that he is developing and growing at an OK rate; but mostly because we actually get some positive feedback from spending time with him!
(2) He seems much more aware of his hands and reaches for things with intent. Also, he is able to hold his "kung-fu grip" on something for an extended period of time. It's nice when he holds my finger!
(3) He also seems much more aware of his environment. He will follow us with his eyes as we move about the room.
(4) He is more comfortable with being held. This is still an ongoing issue. We want him to see being held by us as a source of comfort. He is getting there.
(5) He is talking! OK, he is not saying words, or even really syllables. But he is making a lot of sounds and he keeps doing it. I am sure that this is the precursor of learning to talk.
We still have a lot of work to do with regards to getting him comfortable on his stomach ("tummy time", they call it), as well as getting him to the point of being able to roll over and eventually sit up. Always another goal to progress toward!
OK, on to Ann. She has really taken to motherhood and is enjoying her time at home with Zupe. She is the major care-giver, while I am basically the "bread-winner" who helps out as I can when I am home. It is funny how I studied traditional gender roles while at university and thought "my life will be different"; and here I am living in the 1960s (well, kind of). We have been helped in the loss of half of our house's income by the fact that Australia offers 18 weeks of paid parental leave (at minimum wage), as well as a small carer's allowance to help with Zuperfliegen needing oxygen. The government also provides all the oxygen for him. This is a country that really does these things right!
Anyway, Ann is happy and healthy and a loving mother.
So what about the fathering side of Zuperfliegen's parenting? Well, if I had written this post two months ago, I think it would have been somewhat despondent. I was having some difficulty with Zupe. It was not that he was crying all the time; he has never suffered from colic. But crying was still pretty much the only sort of communication I was getting from him. He was that guy - you know, the one who is part of your gaming group, but all he ever does is complain and you get kind of tired of it. Combined with his seeming dislike of being held and his inability to smile, I was finding it all a bit depressing.
His partial aversion to being held and what appeared to be slower development and the risk of oxygen deprivation at birth and until he was diagnosed as needing it all fed into one of my greatest fears: that he will be severely autistic or otherwise mentally disabled. If that were to be the case, we would, of course, still love him and do the best we could for him. But, for me, it would be a difficult road to acceptance. Fortunately, his advancements over the past two months have done a lot to allay my fear.
Even if I could get past those two big issues, there was still the difficulty for me that I found Zuperfliegen kind of, well, boring. Sure, I thought he was an amazing miracle of life and super-cute, and I think it would have been fair to say that I loved him, but there just was not all that much to do with him. I mean, he was still working out what those things at the ends of his arms were - his hands - not to mention that they had a relationship to each other! After a number of minutes, I would think, "Time to get back to my computer..." (Of course, if he was crying, that moment came a lot faster.)
What helped a lot - other than the developmental advancements I wrote about above - was altering my expectations of parenting. You see, when I thought about having a child and parenting, my mind would process the data by playing a number of "films" in my head - holding his hand as we crossed the street, playing games on a Sunday afternoon, introducing him to the classic science fiction films, etc. I eventually had to realise that all of those things were years and years away. I had to focus on the here and now, and find the joys present in that. Sure, all this seems really obvious; but it was still quite a revelation for me, and it helped me to start down a much more positive path.
So, nowadays, I feel pretty good about everything. It is nice to see Zuperfliegen responding to his environment and finding joy there. I experienced a moment the other day - I was holding him and he just went crazy with smiling and kicking his legs and thrashing his arms about (some of his main forms of communication) - and that was a fabulous moment for me. My heart just filled with joy and love. I'm looking forward to seeing what happens next!
But I'll still be super-thrilled when I can finally hold his hand as we cross the street, play games with him on a Sunday afternoon, and introduce him to the classic science fiction films...
Let's first talk about Zuperfliegen's health. Overall, I think it is very good. He is eating and growing like a champ. His height and weight are both around the 70th percentile, with his head size a little higher than that (go, big-headed guys!). He is also sleeping through the night, as well as getting a few naps during the day. And today we saw what appears to be the start of his first tooth.
As you may remember, Zuperfliegen suffers from sleep apnea and requires oxygen 24 hours a day. This is a developmental issue and the prognosis is that he will develop out of it by the end of his first year. We are scheduled for a sleep study at the hospital every three months to monitor his progress and, eventually, determine when he can get off the oxygen. Our first sleep study was supposed to be on August 3. Unfortunately, Zupe had caught a cold at that time and the hospital did not want to do the study unless he was completely well. So the sleep study has been rescheduled for September 5. That was a little disappointing, as Ann and I were looking forward to hearing what progress he has made. But we recognise that it was highly unlikely that he was going to come off the oxygen at this point, so we can deal with waiting a little longer to hear about his current status. We do worry a little that this will push all the future sleep studies back a month, also.
Zuperfliegen has been suffering from an advanced case of eczema giving him a sandpaper-y feel to his skin. Ann has been pursuing various solutions, all with minimal effect. The current perspective, from Zupe's general practitioner, is that it is an allergic response triggered by the season (as it is winter here, the air is dry and cold). So she prescribed a standard moisturizer for babies, a strong steroidal topical cream, bath oil instead of soap, and the removal of gluten and dairy from the food Ann eats (as well as switching the formula for Zupe). We are hoping this, combined with the eventual change of season and warming of the days, will resolve the issue (and that we are eventually able to work gluten and dairy back into Ann's diet!).
The big news about Zuperfliegen is that we have been able to observe developmental changes:
(1) He is smiling! That has really made a big difference. Partly because it means that he is developing and growing at an OK rate; but mostly because we actually get some positive feedback from spending time with him!
(2) He seems much more aware of his hands and reaches for things with intent. Also, he is able to hold his "kung-fu grip" on something for an extended period of time. It's nice when he holds my finger!
(3) He also seems much more aware of his environment. He will follow us with his eyes as we move about the room.
(4) He is more comfortable with being held. This is still an ongoing issue. We want him to see being held by us as a source of comfort. He is getting there.
(5) He is talking! OK, he is not saying words, or even really syllables. But he is making a lot of sounds and he keeps doing it. I am sure that this is the precursor of learning to talk.
We still have a lot of work to do with regards to getting him comfortable on his stomach ("tummy time", they call it), as well as getting him to the point of being able to roll over and eventually sit up. Always another goal to progress toward!
OK, on to Ann. She has really taken to motherhood and is enjoying her time at home with Zupe. She is the major care-giver, while I am basically the "bread-winner" who helps out as I can when I am home. It is funny how I studied traditional gender roles while at university and thought "my life will be different"; and here I am living in the 1960s (well, kind of). We have been helped in the loss of half of our house's income by the fact that Australia offers 18 weeks of paid parental leave (at minimum wage), as well as a small carer's allowance to help with Zuperfliegen needing oxygen. The government also provides all the oxygen for him. This is a country that really does these things right!
Anyway, Ann is happy and healthy and a loving mother.
So what about the fathering side of Zuperfliegen's parenting? Well, if I had written this post two months ago, I think it would have been somewhat despondent. I was having some difficulty with Zupe. It was not that he was crying all the time; he has never suffered from colic. But crying was still pretty much the only sort of communication I was getting from him. He was that guy - you know, the one who is part of your gaming group, but all he ever does is complain and you get kind of tired of it. Combined with his seeming dislike of being held and his inability to smile, I was finding it all a bit depressing.
His partial aversion to being held and what appeared to be slower development and the risk of oxygen deprivation at birth and until he was diagnosed as needing it all fed into one of my greatest fears: that he will be severely autistic or otherwise mentally disabled. If that were to be the case, we would, of course, still love him and do the best we could for him. But, for me, it would be a difficult road to acceptance. Fortunately, his advancements over the past two months have done a lot to allay my fear.
Even if I could get past those two big issues, there was still the difficulty for me that I found Zuperfliegen kind of, well, boring. Sure, I thought he was an amazing miracle of life and super-cute, and I think it would have been fair to say that I loved him, but there just was not all that much to do with him. I mean, he was still working out what those things at the ends of his arms were - his hands - not to mention that they had a relationship to each other! After a number of minutes, I would think, "Time to get back to my computer..." (Of course, if he was crying, that moment came a lot faster.)
What helped a lot - other than the developmental advancements I wrote about above - was altering my expectations of parenting. You see, when I thought about having a child and parenting, my mind would process the data by playing a number of "films" in my head - holding his hand as we crossed the street, playing games on a Sunday afternoon, introducing him to the classic science fiction films, etc. I eventually had to realise that all of those things were years and years away. I had to focus on the here and now, and find the joys present in that. Sure, all this seems really obvious; but it was still quite a revelation for me, and it helped me to start down a much more positive path.
So, nowadays, I feel pretty good about everything. It is nice to see Zuperfliegen responding to his environment and finding joy there. I experienced a moment the other day - I was holding him and he just went crazy with smiling and kicking his legs and thrashing his arms about (some of his main forms of communication) - and that was a fabulous moment for me. My heart just filled with joy and love. I'm looking forward to seeing what happens next!
But I'll still be super-thrilled when I can finally hold his hand as we cross the street, play games with him on a Sunday afternoon, and introduce him to the classic science fiction films...
Friday 29 April 2011
A Song For Zuperfliegen
Ann recently posted a couple of songs for Zupe on her blog. You can find them here and here. So I thought I should share a song that has meant a lot to me for many years - well before I ever thought I would have a child, in fact.
It was written by David Bowie for his newly-born son, Zowie (or, more fully, Duncan Zowie Hayward Jones) and I think it's beautiful.
Interestingly, little Zowie grew up to be Duncan Jones, the successful film director of the excellent science fiction film, Moon, and the more-recent and also excellent Source Code.
Also interestingly, Duncan attended the College of Wooster in Ohio while Ann was a professor there. David Bowie attended the graduation ceremony (of course).
Zowie, Zuperfliegen - both 'Z' names. Lots of conceptual connections!
Anyway, here's another (slightly different) version of the song, which was the first public performance. It's from the John Peel Show, June 1971.
It was written by David Bowie for his newly-born son, Zowie (or, more fully, Duncan Zowie Hayward Jones) and I think it's beautiful.
Interestingly, little Zowie grew up to be Duncan Jones, the successful film director of the excellent science fiction film, Moon, and the more-recent and also excellent Source Code.
Also interestingly, Duncan attended the College of Wooster in Ohio while Ann was a professor there. David Bowie attended the graduation ceremony (of course).
Zowie, Zuperfliegen - both 'Z' names. Lots of conceptual connections!
Anyway, here's another (slightly different) version of the song, which was the first public performance. It's from the John Peel Show, June 1971.
He Is Risen! He Is Coming (Home)!
(Continuing with the Easter theme...)
It's A Miracle!
All the people and governmental agencies required to collaborate and work for the arrangement of the oxygen-at-home program and Zuperfliegen's release from the hospital were able to do so in an amazingly short period of time. It's the morning of Friday, 29 April - exactly three weeks after his birth - and the oxygen has been delivered to our home. I will soon be making arrangements to pick up Ann and Zuperfliegen from the hospital and bring them back home to resume our life as a New Family.
The Next Stage is about to begin!
In celebration, I once again share the movie poster - now in it's slightly revised and final form - put together by our amazing friend, Ben Nelson:
It's A Miracle!
All the people and governmental agencies required to collaborate and work for the arrangement of the oxygen-at-home program and Zuperfliegen's release from the hospital were able to do so in an amazingly short period of time. It's the morning of Friday, 29 April - exactly three weeks after his birth - and the oxygen has been delivered to our home. I will soon be making arrangements to pick up Ann and Zuperfliegen from the hospital and bring them back home to resume our life as a New Family.
The Next Stage is about to begin!
In celebration, I once again share the movie poster - now in it's slightly revised and final form - put together by our amazing friend, Ben Nelson:
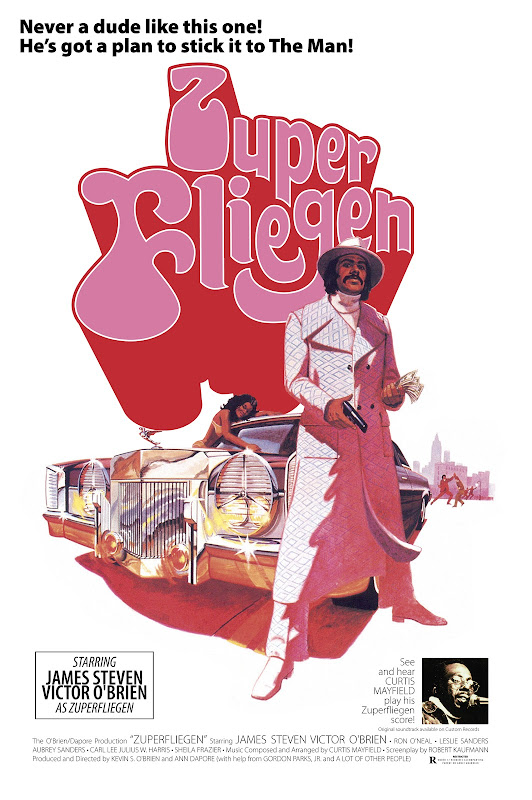 |
| From Zuperfliegen |
Update on the ongoing Zuperfliegen Experience
But first, are you experienced?
Have you ever been experienced?
Well, I have.
- Jimi Hendrix, "Are You Experienced?"
NOTE: This post is a little weird with regards to time. I started composing it on 16 April - 8 days after Zuperfliegen's birth. But I didn't get it completed and posted on that day; so time moved on and things changed and on 25 April I revised what I had written. But I still didn't get it completed and posted and time moved on and things changed again. It's now the morning of Friday, 29 April - three weeks after Zuperfliegen's birth. So I'm going to finish the post I would have completed on 25 April and that's what you're reading here. I'll follow this with a new post that will bring us up to date. So, back to 25 April:
Hey, Happy Easter! I'm not particularly religious any more - and I consider myself more of a Taoist than a Christian - but in my current troubled times, I find "He Is Risen" to be an uplifting, hopeful thought.
(I'm starting this message in the late evening of Monday, 25 April. Technically, Easter has come and gone - even in the USA - but Australia has Easter Monday (!) as a public holiday. Except this year, because ANZAC Day (kind of like Veterans' Day in the USA) has to fall on the 25th, the public holiday of Easter Monday will be observed on Tuesday! So I think it's still OK to say "Happy Easter".)
I'm not exactly known for prompt correspondence - which I discussed in a previous blog entry - but I've gone even more "radio silent" lately. It's really just a matter of spending so much time on Zuperfliegen - traveling to and from the hospital and spending time with him, trying to take care of what needs to be done for the future, and just plain worrying. Almost everything else has been pushed aside to be dealt with "later".
The Status As Of Right Now: Today was Zuperfliegen's 17th day out in the world, but he's never left the hospital. Ann was discharged from the hospital on 14 April and she and I came home, but Zuperfliegen had to remain in the Neonatal Urgent Care Unit (which probably makes things sound worse than they actually are). The doctors have concluded he has "dysrythmic breathing" and sleep apnea. He has moments when he stops breathing while sleeping, which reduces the level of oxygen in his blood to inappropriate levels. When he comes home, he will have to be on oxygen all the time; so we'll get to deal with that on top of the challenges of being new parents to an infant. The oxygen will be required for at least six months, and possibly for a year or more.
As the hospital has done the testing they need to do, he's ready to come home. But that can't happen until the oxygen-at-home situation is set up; and that can't happen until the bureaucratic wheels grind a little; and that can't happen until Australia opens for business again. (Since Good Friday, Easter Sunday, Easter Monday and ANZAC Day are all public holidays, Australia is experiencing a five-day weekend. That's great for most people, but is just a big hold-up for me and Ann this year.) We'll try to finalise arrangements this Wednesday (27 April) and are hopeful that Zuperfliegen will be able to come home on Thursday or Friday. But there's no guarantee that will happen and it may be next week before he makes it out of the hospital (which means that he would come home after I return to work, despite taking all of April off work to help Ann cope with the new situation). And, "next week" means Tuesday, at the earliest, because Monday (2 May) is yet another public holiday (Labour Day)!
Zupe's problem lies in his brain rather than his lungs. The doctors see this condition a few times each year - though it is more common in premature babies. He keeps getting compared to premature babies, despite the fact that he was born a week after his due date! Many babies mature out of it, and that's what we hope will happen during the 6-12 months he's on the oxygen. However, some children have additional brain abnormalities and/or developmental issues; but these typically cannot be determined until the brain cortex develops more over the next three years. So, we hope that everything will work out fine in the end - and that is an entirely possible outcome - but it's also possible that we'll have more unpleasant news over the next three years.
For news of a more positive bend, I can report that he has surpassed his birth weight and is eating like a champ. He wakes every three to four hours and requests - sometimes quite vehemently - to be fed. This is quite different from his earlier days, and all in a good way. In fact, the amount he has developed in the past two-and-a-half weeks is amazing - and very encouraging! He is alert and seems to be responding to his environment.
A Bit More Of The Story Of How We Got Here: We were originally due to be discharged on 13 April. However, Zuperfliegen had been having difficulty with feeding. He wasn't really taking to breastfeeding (which the hospital strongly encouraged and Ann and I decided was best for him). But we figured that was a process of learning, both on his part and Ann's. Because his need for food was increasing every day (as he grew), we put him on a feeding schedule where Ann would try to breastfeed him and then we would give him breast milk (which Ann had expressed earlier) and then top it up with formula, to make sure he was getting his "quota".
Originally, this was intended to happen every three hours (around the clock)! But since the process could easily take 1.5-2 hours - leaving us (mainly Ann!) only an hour or so to rest/sleep before starting again - we quickly moved it to an "every four hours" schedule. (And even that's pretty crazy!) But the biggest issue was that Zuperfliegen was sleepy/sluggish almost all of the time. Typically, you can just wait for your baby to cry to indicate that it's hungry; but, he had never done that. (He's super-relaxed and quiet, which is great...except that it creates a potentially huge problem with regards to making sure he gets enough food!) So the first part of every session would be rousing Zupe from his slumber, which would often be a difficult and prolonged affair - making it even harder to keep to his necessary feeding schedule.
As you can probably imagine, this was really stressing out me and Ann. We began to think more strongly that something was wrong; mainly because we just couldn't see this feeding pattern as tenable. Much consternation was expressed to the midwives that were attending to us. Eventually, a monitor was attached that measured his pulse and percentage of necessary oxygen in the blood. The latter was frequently dropping to the 80s when you want it to be 100 percent (or at least 95 or higher). More worry, as fears of brain damage and other problems entered our minds. Our paediatrician (I just can't get used to the Australian/British spelling of that word...) felt the situation was OK and just that some babies tend to be a bit sleepy/sluggish and slow on oxygen uptake for several days, but get up to speed as they continue to develop. It was very hard for us to accept this idea, though, as we were due to be discharged (and on our own) the following morning.
Our anguish convinced the midwives and/or paediatrician to call in a pulmonary/respiratory specialist for a consultation. He shared our concerns about the blood-oxygen levels (SpO2 levels, where the "2" should be subscripted, as O2 represents oxygen) and suggested Zuperfliegen be transferred to the Neonatal Urgent Care Unit for overnight observation and extended recording of vital signs, which he was. Though Ann and I were certainly worried about the possible implications of Zupe's condition, we were greatly relieved that our worries were being acknowledged and our child would be receiving much greater attention to his condition. This also meant that Ann and I were given an evening "off" after four days of sleep deprivation and stress.
Zuperfliegen's Sp02 levels overnight (Wednesday-Thursday) tended to trend to the low 90s, and thus lower than we would like. It was decided to do further testing to see if a reason could be found. Over Thursday and Friday, ultrasounds were taken of his heart and his head/brain, an x-ray was taken of his lungs, and various blood tests were conducted. Everything came up normal! In addition, he looked fine and acted fine (albeit sleeping a lot; though babies do that).
The next big (and possibly final) step was to put him in an overnight sleep study. Those are generally scheduled well in advance, so they had to give us "emergency" priority to get us in two days later. Ann stayed overnight with Zuperfliegen after he was hooked up with a bunch of sensors - EEG and ECG and other measurements. That data produced the diagnosis of "dysrythmic breathing" and sleep apnea and confirmed that he would have to be sent home on oxygen. Which meant that we needed to apply through Centrelink (kind of like the Welfare Office in the USA, but more common and acceptable in this more socialist environment) to get the payment in place for the oxygen service so that we could then get it delivered so that we could take Zuperfliegen home. But, as that diagnosis/decision came about just before this long Good Friday to Easter Monday/Tuesday break, there is nothing we can do for five days but wait to fill out and complete the forms on Wednesday when the world starts up again. And, of course, we're spending the days visiting and caring for Zuperfliegen in the hospital.
How I Feel About All This: It's a real rollercoaster of ambivalence! When I first found out about the problem, my mood was very dark. One of my greatest fears regarding having a child is the possibility of serious mental damage that would mean he would need to be cared for all his life. The possibility of that happening with Zuperfliegen touches upon areas of serious fear/depression/despair in my mind.
As time passes, however, I work toward a more realistic/workable (I hope) perspective. I realise that there is always the possibility of A Bad Thing (or Things) happening, but hope and joy and love seem to persist and, generally, things turn out "OK". Or, as I have said/believed for many years: "Life sucks, but is mostly worth living." And it's this overall-weighted-to-the-positive perspective that allowed me to decide to have a child in the first place.
Ann and I are, of course, disappointed that Zuperfliegen has this additional challenge (which means that we have an additional challenge, too). But we are significantly buoyed by his continued development and otherwise good health. So far, it seems that, except for the oxygen/breathing/sleep apnea thing, he's a pretty "normal" boy. And, of course, things could always be much, much worse.
We're also happy that his condition was caught and diagnosed and is being treated. It frightens us how close we came to just being sent home and having things develop without this intervention! The additional ten-plus days of having to travel to and from the hospital has been a drag, but far better than the alternative.
A few other things we're thankful for: The staff of the Mater Mathers' Hospital has been incredibly kind, helpful and competent. It's hard to underestimate how important that is in areas of health! We're also thrilled that we live in a country with an excellent Medicare system and private insurance companies that seem to be very reasonable/supportive (and we don't feel that we have to fight for our claims to be paid; in fact, it all seems to be happening automatically, with the hospital dealing directly with our insurance company). And, it's wonderful that Australia provides 18 weeks of paid parental leave (admittedly, it's minimum wage; but every little bit helps now that we are down to one income) and a year of unpaid parental leave (so that Ann can provide the care Zuperfliegen needs and then eventually return to her job). Socialism is a Good Thing! I'm also thankful that I was able to take all of April off as a "holiday" (ahem) from work and was thus able to focus on these events. (Thanks, Tom and New Horizons!)
We continue to look forward to Zuperfliegen actually coming home....
Have you ever been experienced?
Well, I have.
- Jimi Hendrix, "Are You Experienced?"
NOTE: This post is a little weird with regards to time. I started composing it on 16 April - 8 days after Zuperfliegen's birth. But I didn't get it completed and posted on that day; so time moved on and things changed and on 25 April I revised what I had written. But I still didn't get it completed and posted and time moved on and things changed again. It's now the morning of Friday, 29 April - three weeks after Zuperfliegen's birth. So I'm going to finish the post I would have completed on 25 April and that's what you're reading here. I'll follow this with a new post that will bring us up to date. So, back to 25 April:
Hey, Happy Easter! I'm not particularly religious any more - and I consider myself more of a Taoist than a Christian - but in my current troubled times, I find "He Is Risen" to be an uplifting, hopeful thought.
(I'm starting this message in the late evening of Monday, 25 April. Technically, Easter has come and gone - even in the USA - but Australia has Easter Monday (!) as a public holiday. Except this year, because ANZAC Day (kind of like Veterans' Day in the USA) has to fall on the 25th, the public holiday of Easter Monday will be observed on Tuesday! So I think it's still OK to say "Happy Easter".)
I'm not exactly known for prompt correspondence - which I discussed in a previous blog entry - but I've gone even more "radio silent" lately. It's really just a matter of spending so much time on Zuperfliegen - traveling to and from the hospital and spending time with him, trying to take care of what needs to be done for the future, and just plain worrying. Almost everything else has been pushed aside to be dealt with "later".
The Status As Of Right Now: Today was Zuperfliegen's 17th day out in the world, but he's never left the hospital. Ann was discharged from the hospital on 14 April and she and I came home, but Zuperfliegen had to remain in the Neonatal Urgent Care Unit (which probably makes things sound worse than they actually are). The doctors have concluded he has "dysrythmic breathing" and sleep apnea. He has moments when he stops breathing while sleeping, which reduces the level of oxygen in his blood to inappropriate levels. When he comes home, he will have to be on oxygen all the time; so we'll get to deal with that on top of the challenges of being new parents to an infant. The oxygen will be required for at least six months, and possibly for a year or more.
As the hospital has done the testing they need to do, he's ready to come home. But that can't happen until the oxygen-at-home situation is set up; and that can't happen until the bureaucratic wheels grind a little; and that can't happen until Australia opens for business again. (Since Good Friday, Easter Sunday, Easter Monday and ANZAC Day are all public holidays, Australia is experiencing a five-day weekend. That's great for most people, but is just a big hold-up for me and Ann this year.) We'll try to finalise arrangements this Wednesday (27 April) and are hopeful that Zuperfliegen will be able to come home on Thursday or Friday. But there's no guarantee that will happen and it may be next week before he makes it out of the hospital (which means that he would come home after I return to work, despite taking all of April off work to help Ann cope with the new situation). And, "next week" means Tuesday, at the earliest, because Monday (2 May) is yet another public holiday (Labour Day)!
Zupe's problem lies in his brain rather than his lungs. The doctors see this condition a few times each year - though it is more common in premature babies. He keeps getting compared to premature babies, despite the fact that he was born a week after his due date! Many babies mature out of it, and that's what we hope will happen during the 6-12 months he's on the oxygen. However, some children have additional brain abnormalities and/or developmental issues; but these typically cannot be determined until the brain cortex develops more over the next three years. So, we hope that everything will work out fine in the end - and that is an entirely possible outcome - but it's also possible that we'll have more unpleasant news over the next three years.
For news of a more positive bend, I can report that he has surpassed his birth weight and is eating like a champ. He wakes every three to four hours and requests - sometimes quite vehemently - to be fed. This is quite different from his earlier days, and all in a good way. In fact, the amount he has developed in the past two-and-a-half weeks is amazing - and very encouraging! He is alert and seems to be responding to his environment.
A Bit More Of The Story Of How We Got Here: We were originally due to be discharged on 13 April. However, Zuperfliegen had been having difficulty with feeding. He wasn't really taking to breastfeeding (which the hospital strongly encouraged and Ann and I decided was best for him). But we figured that was a process of learning, both on his part and Ann's. Because his need for food was increasing every day (as he grew), we put him on a feeding schedule where Ann would try to breastfeed him and then we would give him breast milk (which Ann had expressed earlier) and then top it up with formula, to make sure he was getting his "quota".
Originally, this was intended to happen every three hours (around the clock)! But since the process could easily take 1.5-2 hours - leaving us (mainly Ann!) only an hour or so to rest/sleep before starting again - we quickly moved it to an "every four hours" schedule. (And even that's pretty crazy!) But the biggest issue was that Zuperfliegen was sleepy/sluggish almost all of the time. Typically, you can just wait for your baby to cry to indicate that it's hungry; but, he had never done that. (He's super-relaxed and quiet, which is great...except that it creates a potentially huge problem with regards to making sure he gets enough food!) So the first part of every session would be rousing Zupe from his slumber, which would often be a difficult and prolonged affair - making it even harder to keep to his necessary feeding schedule.
As you can probably imagine, this was really stressing out me and Ann. We began to think more strongly that something was wrong; mainly because we just couldn't see this feeding pattern as tenable. Much consternation was expressed to the midwives that were attending to us. Eventually, a monitor was attached that measured his pulse and percentage of necessary oxygen in the blood. The latter was frequently dropping to the 80s when you want it to be 100 percent (or at least 95 or higher). More worry, as fears of brain damage and other problems entered our minds. Our paediatrician (I just can't get used to the Australian/British spelling of that word...) felt the situation was OK and just that some babies tend to be a bit sleepy/sluggish and slow on oxygen uptake for several days, but get up to speed as they continue to develop. It was very hard for us to accept this idea, though, as we were due to be discharged (and on our own) the following morning.
Our anguish convinced the midwives and/or paediatrician to call in a pulmonary/respiratory specialist for a consultation. He shared our concerns about the blood-oxygen levels (SpO2 levels, where the "2" should be subscripted, as O2 represents oxygen) and suggested Zuperfliegen be transferred to the Neonatal Urgent Care Unit for overnight observation and extended recording of vital signs, which he was. Though Ann and I were certainly worried about the possible implications of Zupe's condition, we were greatly relieved that our worries were being acknowledged and our child would be receiving much greater attention to his condition. This also meant that Ann and I were given an evening "off" after four days of sleep deprivation and stress.
Zuperfliegen's Sp02 levels overnight (Wednesday-Thursday) tended to trend to the low 90s, and thus lower than we would like. It was decided to do further testing to see if a reason could be found. Over Thursday and Friday, ultrasounds were taken of his heart and his head/brain, an x-ray was taken of his lungs, and various blood tests were conducted. Everything came up normal! In addition, he looked fine and acted fine (albeit sleeping a lot; though babies do that).
The next big (and possibly final) step was to put him in an overnight sleep study. Those are generally scheduled well in advance, so they had to give us "emergency" priority to get us in two days later. Ann stayed overnight with Zuperfliegen after he was hooked up with a bunch of sensors - EEG and ECG and other measurements. That data produced the diagnosis of "dysrythmic breathing" and sleep apnea and confirmed that he would have to be sent home on oxygen. Which meant that we needed to apply through Centrelink (kind of like the Welfare Office in the USA, but more common and acceptable in this more socialist environment) to get the payment in place for the oxygen service so that we could then get it delivered so that we could take Zuperfliegen home. But, as that diagnosis/decision came about just before this long Good Friday to Easter Monday/Tuesday break, there is nothing we can do for five days but wait to fill out and complete the forms on Wednesday when the world starts up again. And, of course, we're spending the days visiting and caring for Zuperfliegen in the hospital.
How I Feel About All This: It's a real rollercoaster of ambivalence! When I first found out about the problem, my mood was very dark. One of my greatest fears regarding having a child is the possibility of serious mental damage that would mean he would need to be cared for all his life. The possibility of that happening with Zuperfliegen touches upon areas of serious fear/depression/despair in my mind.
As time passes, however, I work toward a more realistic/workable (I hope) perspective. I realise that there is always the possibility of A Bad Thing (or Things) happening, but hope and joy and love seem to persist and, generally, things turn out "OK". Or, as I have said/believed for many years: "Life sucks, but is mostly worth living." And it's this overall-weighted-to-the-positive perspective that allowed me to decide to have a child in the first place.
Ann and I are, of course, disappointed that Zuperfliegen has this additional challenge (which means that we have an additional challenge, too). But we are significantly buoyed by his continued development and otherwise good health. So far, it seems that, except for the oxygen/breathing/sleep apnea thing, he's a pretty "normal" boy. And, of course, things could always be much, much worse.
We're also happy that his condition was caught and diagnosed and is being treated. It frightens us how close we came to just being sent home and having things develop without this intervention! The additional ten-plus days of having to travel to and from the hospital has been a drag, but far better than the alternative.
A few other things we're thankful for: The staff of the Mater Mathers' Hospital has been incredibly kind, helpful and competent. It's hard to underestimate how important that is in areas of health! We're also thrilled that we live in a country with an excellent Medicare system and private insurance companies that seem to be very reasonable/supportive (and we don't feel that we have to fight for our claims to be paid; in fact, it all seems to be happening automatically, with the hospital dealing directly with our insurance company). And, it's wonderful that Australia provides 18 weeks of paid parental leave (admittedly, it's minimum wage; but every little bit helps now that we are down to one income) and a year of unpaid parental leave (so that Ann can provide the care Zuperfliegen needs and then eventually return to her job). Socialism is a Good Thing! I'm also thankful that I was able to take all of April off as a "holiday" (ahem) from work and was thus able to focus on these events. (Thanks, Tom and New Horizons!)
We continue to look forward to Zuperfliegen actually coming home....
Saturday 9 April 2011
The Zuperfliegen Birth Photos
Ann and Kevin, just before the cesarean delivery began:
Kevin and Zuperfliegen just after the birth, weighing and a little bit of clean-up:
Followed by Ann finally able to see her new son!
Ann, just after the delivery, in the post-op recovery room:
Day #2 (his first full day) - Awake and aware!
We're a happy family!
 |
| From Zuperfliegen |
Kevin and Zuperfliegen just after the birth, weighing and a little bit of clean-up:
 |
| From Zuperfliegen |
Followed by Ann finally able to see her new son!
 |
| From Zuperfliegen |
Ann, just after the delivery, in the post-op recovery room:
 |
| From Zuperfliegen |
Day #2 (his first full day) - Awake and aware!
 |
| From Zuperfliegen |
We're a happy family!
 |
| From Zuperfliegen |
Friday 8 April 2011
The Ongoing Birth Of Zuperfliegen Baadasssss O'Brien!
Friday, 8 April, 2011 (Zuperfliegen's 41-week anniversary of embryo to fetus)
(All times are Brisbane Time)
Earlier this week, we decided to induce labour (Australian spelling) on Friday or the weekend if a space could be found at the hospital (Mater Mothers Private Hospital in South Brisbane). Yesterday we were told that there was an opening on Friday (today).
7:30 AM - We got to the hospital for our 7:00 appointment. Just a little too much to do in the morning, so we had not left on time...
8:30 AM - The doctor arrives. (Guess it wasn't such a problem that we were late...) Ann is dilated to 3 cm and fully effaced. Her waters are "broken" and they start the administration of syntocinon. Afterwards, Kevin is exhausted from not getting enough sleep last night - trying to get too much stuff done on the computer in preparation of leaving home for four days - so he takes a nap in the chair. (First step of any big project: take a nap!)
10:00 AM - Kevin wakes up, feeling totally refreshed. Ann is having mild contractions every three minutes.
11:00 AM - Ann says "It hurts." (But she's really taking it well, I think!)
11:15 AM - Ann says "I'm no longer smiling...!" Things are getting serious. Time for Kevin to get off the damn computer!
11:45 AM - Ann is feeling a lot of pain. Only 4 cm dilation. Drat! An epidural is requested.
12:01 PM - The epidural is applied. A short time later, Ann is feeling much better (that is, much less pain). Now it looks like we just have to wait a number of hours before something else happens. Kevin eats some lunch. Ann's not feeling hungry.
1:00 PM - Time for a nap for Ann. Kevin will either browse the web or nap, also.
(And then it took me about six hours to get back to the computer to tell the rest of the story...)
1:30 PM - Ann is relaxing and I'm doing web/blog stuff. I frequently look up to check on the monitor showing Zuperfliegen's heart rate. I notice that he keeps going down below the preferred range (110-160 beats per minute). I point it out to the midwife, who has already noticed it. She has Ann try a variety of positions as that often affects heart rate. Nothing really seems to make a big difference. There's a thought that maybe Ann has rushed to the next stage. The midwife does an exam and declares that Ann is almost entirely dilated at 9 cm! Golly! About this time, the doctor comes in and does another exam. The issue is that Zupe hasn't moved down into the pelvis as far as he needs to - probably because of his "freakishly large head" (true) - and the level of syntocinon seems to be stressing him.
1:45 PM - The doctor decides that we need to move to an emergency cesarean! Suddenly, the room is awash with a bunch of new people, all moving very quickly! I see Zupe's heart rate "crash" a couple of times - which was scary - though it's not clear what's happening because they are also disconnecting Ann from the monitors. Ann needs to sign a consent form; I read it over quickly, just to be sure. (It was all fine.)
2:00 PM (or thereabouts) - Ann (bed and all) is wheeled from the room to the operating theatre. I'm rushed along, as I'm able to be with her during the operation, but I have to quickly grab any valuables (like this laptop) to store in a locker, as well as change into sterile scrubs. When I eventually get into the room, they are about to start. I'm given a chair by Ann's head. She's totally conscious, because they're using a local anaesthesia for the lower part of her body. They put a sterile cloth screen up below her neck and we're not able to see anything! I feel disappointed, as I was looking forward to the new "life experience" of witnessing a live operation. Overall, the event is scary for Ann and I - things are moving fast and there's a lot at stake - but we reminded ourselves that C-sections are done all the time, frequently as voluntary procedures.
2:47 PM - NEVER A DUDE LIKE THIS ONE!
Ladies and Gentlemen of The World, I present to you: Zuperfliegen Baadassss O'Brien!
Legal Name: James Steven Victor O'Brien
(obviously, it was, indeed, a boy!)
Weight: 3340 grams (about 7 pounds, 6 ounces)
Length: 54 cm (21.25 inches)
Head Circumference: 38 cm (15 inches; "freakishly large")
Wow, babies are messy-looking when they first come out. My first thought was "blood-covered zombie!" Nonetheless, he cleaned up nicely and got a 6 (out of 10) on the APGAR scale upon emergence and then a 9 after he was pampered a bit by the paediatrician. Apparently, no one ever gets a 10... In the 90th percentile already; that's my boy!
THEN, A LITTLE LATER - We got whisked out of the operating room fairly quickly. Then we just hung out in the post-op for a little while, as Zuperfliegen and Ann were looked after - checking that they were recovering nicely from the procedure (which they were). After about an hour, we were taken up to our (private; yay!) room.
Mother and son (and father) are all apparently healthy and feeling OK! (As of 8:30 PM, anyway.)
And so The Adventure continues!
(Pictures to be posted tomorrow in a new, separate blog entry, most likely.)
(All times are Brisbane Time)
Earlier this week, we decided to induce labour (Australian spelling) on Friday or the weekend if a space could be found at the hospital (Mater Mothers Private Hospital in South Brisbane). Yesterday we were told that there was an opening on Friday (today).
7:30 AM - We got to the hospital for our 7:00 appointment. Just a little too much to do in the morning, so we had not left on time...
8:30 AM - The doctor arrives. (Guess it wasn't such a problem that we were late...) Ann is dilated to 3 cm and fully effaced. Her waters are "broken" and they start the administration of syntocinon. Afterwards, Kevin is exhausted from not getting enough sleep last night - trying to get too much stuff done on the computer in preparation of leaving home for four days - so he takes a nap in the chair. (First step of any big project: take a nap!)
10:00 AM - Kevin wakes up, feeling totally refreshed. Ann is having mild contractions every three minutes.
11:00 AM - Ann says "It hurts." (But she's really taking it well, I think!)
11:15 AM - Ann says "I'm no longer smiling...!" Things are getting serious. Time for Kevin to get off the damn computer!
11:45 AM - Ann is feeling a lot of pain. Only 4 cm dilation. Drat! An epidural is requested.
12:01 PM - The epidural is applied. A short time later, Ann is feeling much better (that is, much less pain). Now it looks like we just have to wait a number of hours before something else happens. Kevin eats some lunch. Ann's not feeling hungry.
1:00 PM - Time for a nap for Ann. Kevin will either browse the web or nap, also.
(And then it took me about six hours to get back to the computer to tell the rest of the story...)
1:30 PM - Ann is relaxing and I'm doing web/blog stuff. I frequently look up to check on the monitor showing Zuperfliegen's heart rate. I notice that he keeps going down below the preferred range (110-160 beats per minute). I point it out to the midwife, who has already noticed it. She has Ann try a variety of positions as that often affects heart rate. Nothing really seems to make a big difference. There's a thought that maybe Ann has rushed to the next stage. The midwife does an exam and declares that Ann is almost entirely dilated at 9 cm! Golly! About this time, the doctor comes in and does another exam. The issue is that Zupe hasn't moved down into the pelvis as far as he needs to - probably because of his "freakishly large head" (true) - and the level of syntocinon seems to be stressing him.
1:45 PM - The doctor decides that we need to move to an emergency cesarean! Suddenly, the room is awash with a bunch of new people, all moving very quickly! I see Zupe's heart rate "crash" a couple of times - which was scary - though it's not clear what's happening because they are also disconnecting Ann from the monitors. Ann needs to sign a consent form; I read it over quickly, just to be sure. (It was all fine.)
2:00 PM (or thereabouts) - Ann (bed and all) is wheeled from the room to the operating theatre. I'm rushed along, as I'm able to be with her during the operation, but I have to quickly grab any valuables (like this laptop) to store in a locker, as well as change into sterile scrubs. When I eventually get into the room, they are about to start. I'm given a chair by Ann's head. She's totally conscious, because they're using a local anaesthesia for the lower part of her body. They put a sterile cloth screen up below her neck and we're not able to see anything! I feel disappointed, as I was looking forward to the new "life experience" of witnessing a live operation. Overall, the event is scary for Ann and I - things are moving fast and there's a lot at stake - but we reminded ourselves that C-sections are done all the time, frequently as voluntary procedures.
2:47 PM - NEVER A DUDE LIKE THIS ONE!
Ladies and Gentlemen of The World, I present to you: Zuperfliegen Baadassss O'Brien!
Legal Name: James Steven Victor O'Brien
(obviously, it was, indeed, a boy!)
Weight: 3340 grams (about 7 pounds, 6 ounces)
Length: 54 cm (21.25 inches)
Head Circumference: 38 cm (15 inches; "freakishly large")
Wow, babies are messy-looking when they first come out. My first thought was "blood-covered zombie!" Nonetheless, he cleaned up nicely and got a 6 (out of 10) on the APGAR scale upon emergence and then a 9 after he was pampered a bit by the paediatrician. Apparently, no one ever gets a 10... In the 90th percentile already; that's my boy!
THEN, A LITTLE LATER - We got whisked out of the operating room fairly quickly. Then we just hung out in the post-op for a little while, as Zuperfliegen and Ann were looked after - checking that they were recovering nicely from the procedure (which they were). After about an hour, we were taken up to our (private; yay!) room.
Mother and son (and father) are all apparently healthy and feeling OK! (As of 8:30 PM, anyway.)
And so The Adventure continues!
(Pictures to be posted tomorrow in a new, separate blog entry, most likely.)
Tuesday 5 April 2011
News Flash! - We've added another name!
First: No baby yet. Everybody is happy and healthy, but Zuperfliegen is not yet ready to leave the warm comfort of the womb for the cold joy of the rest of world. It will happen sometime between now and Monday, 11 April; because the doctor will induce labour by then if it does not start naturally. We'll let you know when something happens, of course!
Second: News Flash! We've added another name! (Because we felt that our son didn't have enough already...)
Specifically, we've added a second middle name: Victor. So his full legal name will be James Steven Victor O'Brien. (We're still calling him Zuperfliegen, though!)
There was some discussion about whether Victor should be the first "middle name" or the second. I was torn, because I like the SOB initials (like my own); but, in the end, I felt that Steven deserved the greater prominence.
Victor is in homage to Ann's first cocker spaniel (the one before Zelda). You can read about her great love for him on her blog.
Of course, as a geek, I can't name my son after the dog without thinking about Indiana Jones:
Apparently, Ann and I believe in naming children the same way that cats are named:
T.S. Eliot - The Naming Of Cats
The Naming of Cats is a difficult matter,
It isn't just one of your holiday games;
You may think at first I'm as mad as a hatter
When I tell you, a cat must have THREE DIFFERENT NAMES.
First of all, there's the name that the family use daily,
Such as Peter, Augustus, Alonzo or James,
Such as Victor or Jonathan, George or Bill Bailey--
All of them sensible everyday names.
There are fancier names if you think they sound sweeter,
Some for the gentlemen, some for the dames:
Such as Plato, Admetus, Electra, Demeter--
But all of them sensible everyday names.
But I tell you, a cat needs a name that's particular,
A name that's peculiar, and more dignified,
Else how can he keep up his tail perpendicular,
Or spread out his whiskers, or cherish his pride?
Of names of this kind, I can give you a quorum,
Such as Munkustrap, Quaxo, or Coricopat,
Such as Bombalurina, or else Jellylorum-
Names that never belong to more than one cat.
But above and beyond there's still one name left over,
And that is the name that you never will guess;
The name that no human research can discover--
But THE CAT HIMSELF KNOWS, and will never confess.
When you notice a cat in profound meditation,
The reason, I tell you, is always the same:
His mind is engaged in a rapt contemplation
Of the thought, of the thought, of the thought of his name:
His ineffable effable
Effanineffable
Deep and inscrutable singular Name.
Third: Recently, one of Ann's friends wrote to say that she wanted to make something for Zuperfliegen's room. She asked, "Will the theme be more Beatrix Potter or Winnie-the-Pooh?" We laughed and thought, "umm, it's more like Blaxploitation!" (Though, of the two, Winnie-the-Pooh is way more awesome than Beatrix Potter...)
Along those lines, I wanted to share with you the "official" Zuperfliegen poster, created by our incredibly talented friend, Ben Nelson:
Ah, what an interesting life Zuperfliegen is going to lead!
Second: News Flash! We've added another name! (Because we felt that our son didn't have enough already...)
Specifically, we've added a second middle name: Victor. So his full legal name will be James Steven Victor O'Brien. (We're still calling him Zuperfliegen, though!)
There was some discussion about whether Victor should be the first "middle name" or the second. I was torn, because I like the SOB initials (like my own); but, in the end, I felt that Steven deserved the greater prominence.
Victor is in homage to Ann's first cocker spaniel (the one before Zelda). You can read about her great love for him on her blog.
Of course, as a geek, I can't name my son after the dog without thinking about Indiana Jones:
Apparently, Ann and I believe in naming children the same way that cats are named:
T.S. Eliot - The Naming Of Cats
The Naming of Cats is a difficult matter,
It isn't just one of your holiday games;
You may think at first I'm as mad as a hatter
When I tell you, a cat must have THREE DIFFERENT NAMES.
First of all, there's the name that the family use daily,
Such as Peter, Augustus, Alonzo or James,
Such as Victor or Jonathan, George or Bill Bailey--
All of them sensible everyday names.
There are fancier names if you think they sound sweeter,
Some for the gentlemen, some for the dames:
Such as Plato, Admetus, Electra, Demeter--
But all of them sensible everyday names.
But I tell you, a cat needs a name that's particular,
A name that's peculiar, and more dignified,
Else how can he keep up his tail perpendicular,
Or spread out his whiskers, or cherish his pride?
Of names of this kind, I can give you a quorum,
Such as Munkustrap, Quaxo, or Coricopat,
Such as Bombalurina, or else Jellylorum-
Names that never belong to more than one cat.
But above and beyond there's still one name left over,
And that is the name that you never will guess;
The name that no human research can discover--
But THE CAT HIMSELF KNOWS, and will never confess.
When you notice a cat in profound meditation,
The reason, I tell you, is always the same:
His mind is engaged in a rapt contemplation
Of the thought, of the thought, of the thought of his name:
His ineffable effable
Effanineffable
Deep and inscrutable singular Name.
Third: Recently, one of Ann's friends wrote to say that she wanted to make something for Zuperfliegen's room. She asked, "Will the theme be more Beatrix Potter or Winnie-the-Pooh?" We laughed and thought, "umm, it's more like Blaxploitation!" (Though, of the two, Winnie-the-Pooh is way more awesome than Beatrix Potter...)
Along those lines, I wanted to share with you the "official" Zuperfliegen poster, created by our incredibly talented friend, Ben Nelson:
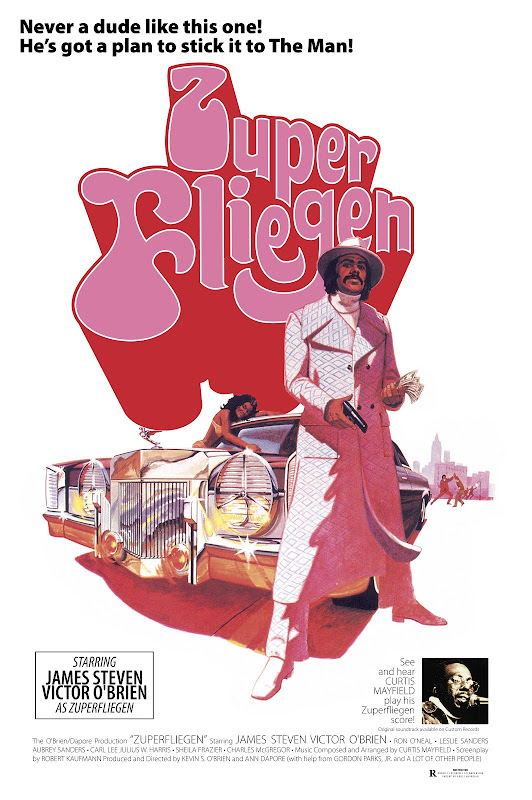 |
| From Zuperfliegen |
Ah, what an interesting life Zuperfliegen is going to lead!
The Missed April Fool
If I were a caring and attentive blogger, I would have posted something on 1 April because (1) it was April Fools Day! and (2) it was the "due date" of Zuperfliegen!
But, in the end, I am what I am and you, Constant Reader, get what you get. And so it goes.
Anyway, no baby yet. We're still waiting. Because we liked the idea of Zuperfliegen coming forth on April Fools' Day - since we missed the opportunity of a cesarian delivery on the Ides of March - we've decided to extend the month of March. So I'm posting this on Tuesday, March 36!
But, in the end, I am what I am and you, Constant Reader, get what you get. And so it goes.
Anyway, no baby yet. We're still waiting. Because we liked the idea of Zuperfliegen coming forth on April Fools' Day - since we missed the opportunity of a cesarian delivery on the Ides of March - we've decided to extend the month of March. So I'm posting this on Tuesday, March 36!
Subscribe to:
Posts (Atom)



